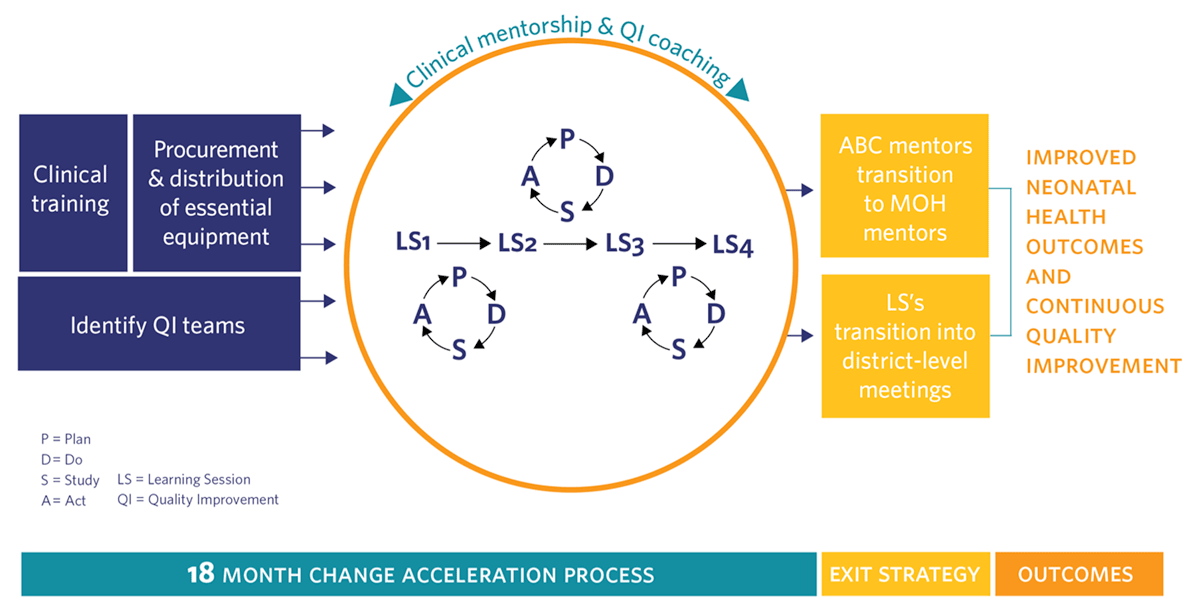
Figure 1
ABC Conceptual Model.
Table 1
Changes in Availability of Essential Medications and Equipment for Kireha (16 facilities) and Southern Kayonza (9 facilities).
| INDICATOR | ABC BASELINE (JUL–SEP 2013) MEDIAN (IQR) | ABC ENDPOINT (JUL–SEP 2015) MEDIAN (IQR) | 12 MONTHS POST INTERVENTION (JUL–SEP 2016) MEDIAN (IQR) | p-VALUE* |
|---|---|---|---|---|
| Percent availability of essential medications for maternal/newborn Care | ||||
| Kirehe | 67 (55–78) | 78 (73–82) | 83 (83–91) | <0.01 |
| S.Kayonza | 35 (25–45) | 83 (75–87) | 87 (75–100) | 0.39 |
| Percent availability of functioning equipment essential for maternal/newborn care | ||||
| Kirehe | 55 (48–64) | 81 (77.8–89) | 89 (89–94) | <0.01 |
| S. Kayonza (N = 9) | 55 (47–56) | 89 (89–94) | 89 (89–94) | 0.4 |
[i] * p-values are for comparisons of end of ABC versus 12 months post-ABC.
Table 2
Changes in Healthcare Coverage and Quality between the end of ABC and 12 months post-ABC.
| INDICATOR | AGGREGATE | SOUTH KAYONZA | KIREHE | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BASELINE (JUL–SEPT 2013) | ABC ENDPOINT (JUL–SEPT 2015) | 12 MONTHS POST-ABC (JUL–SEPT 2016) | P-VALUE COMPARING 12 MONTHS POST-ABC TO ABC ENDPOINT | BASELINE (JUL–SEPT 2013) | ABC ENDPOINT (JUL–SEPT 2015) | 12 MONTHS POST-ABC (JUL–SEPT 2016) | P-VALUE COMPARING 12 MONTHS POST-ABC TO ABC ENDPOINT | BASELINE (JUL–SEPT 2013) | ABC ENDPOINT (JUL–SEPT 2015) | 12 MONTHS POST-ABC (JUL–SEPT 2016) | P-VALUE COMPARING 12 MONTHS POST-ABC TO ABC ENDPOINT | |||
| MEDIAN (IQR) | MEDIAN (IQR) | MEDIAN (IQR) | MEDIAN (IQR) | MEDIAN (IQR) | MEDIAN (IQR) | MEDIAN (IQR) | MEDIAN (IQR) | MEDIAN (IQR) | ||||||
| Percent of deliveries with mothers with 4 or more ANC visits | 13.7 (6.7– 44.2) | 30.4 (15.1–43.1) | 30.9 (23–47) | 0.7 | 42.4 (19.9–47.3) | 36.4 (13.5–66.3) | 53 (24–100) | 0.3 | 10.2 (2.8–26.8) | 29.6 (18–34.2) | 30.7 (20–37) | 0.04 | ||
| Percent of pregnant women delivering in facilities | 89.6 (86.3–94.9) | 92.6 (86.8–95.8) | 95.8 (93–97.4) | 0.0148 | 92.2 (87.2–95.3) | 95.2 (93–96.3) | 96.1 (95.7–98.3) | 0.092 | 88.4 (86.3–96.7) | 91.0 (86.2–94.6) | 94.3 (91–97.2) | 0.06 | ||
| Percent of babies provided immediate skin-to-skin after birth | 53.6 (0–80.9) | 97.4 (96.4–99.3) | 96.2 (86–100) | 0.2 | 91.2 (75.9–100) | 99.6 (96.7–100) | 94.2 (87.7–96.3) | 0.05 | 4.3 (0–53.6) | 97.2 (96.1–98.8) | 96.5 (85.8–100) | 0.8 | ||
| Percent of newborns checked for danger signs within 24 hrs of birth | 46.6 (31.1–96.7) | 98.7 (96.4–100) | 99.3 (89–100) | 0.7 | 52.3 (33.8–98.6) | 100 (93.8–100) | 96.2 86.8–98.8 | 0.01 | 45.7 (15.8–82.1) | 98.6 (97.4–98.8) | 100 (98.2–100) | 0.4 | ||
| Percent women with preterm labor who are treated with antenatal steroids | 0 (0–0) | 41.7 (0–100) | 58 (48–67) | 0.02 | 0 (0–0) | 16.7 (0–33.3) | 54.5 (48.2–86) | 0.03 | 0 (0–0) | 75 (0–100) | 66.6 (62–78) | 0.4 | ||
Table 3
Examples of Ideas for improving the quality of neonatal care that were continued 12 Months after the end of ABC.
| INDICATOR TARGETED | CARE GAP | CHANGE CONCEPT | |
|---|---|---|---|
| Antenatal Care | Percent of Women with 4 ANC visits | 4 ANC visit completion is low because women miss their first ANC appointment | Test women for pregnancy in all departments and transfer for ANC enrollment or same day care if pregnant |
| No mechanism to follow up with women who miss appointments | Make (a) a filing system of medical records or (b) a register modification such that women who miss appointments can be easily recognized and contacted by CHWs | ||
| Women don’t come for ANC because partner is not available | See women for 1st ANC and send her with invitation for her partner to attend following visit | ||
| Delivery Management | Percent of pregnant women delivering in facilities | Women do not deliver at the facility because they fail to do appropriate anticipatory planning | Assist mothers with anticipatory planning of items to have prepared to bring for delivery at their 3rd ANC appointment |
| Percent of women with pPROM treated with antibiotics | Low case identification of women in active preterm labor | Refresher trainings for staff on calculation of gestational age and management of pPROM to improve recognition of labor complications and management | |
| Time to cesarean section | Poor communication and coordination between maternity and neonatal services | Set aside a regularly scheduled time for collaboration between neonatal and maternity services | |
| Post-natal care | Percent of newborns checked for danger signs within 24 hours of birth | Low maternal knowledge and nurse vigilance in checking for neonatal danger signs | Low maternal knowledge and nurse vigilance in checking for neonatal danger signs |
Table 4
Key themes associated with facilitating and challenging factors to ABC sustainability of activities and improvements.
| THEMES | EXAMPLES OF QUOTES |
|---|---|
| Leadership “Buy-In” and “Ownership” | “During the second learning collaborative in Kirehe, the mayor, the vice mayor and the entire leadership team were present. They stayed for the whole day. They took notes and asked questions” I was surprised to see the Mayor sitting there for hours. And you can see that he was very interested and curious to see what is happening. We were feeling supported.” – ABC mentor “…Kabarondo titulaire is a nun. She also a student. She is doing her bachelor degree in nursing, so she is very busy. One day I went to Kabarondo for mentorship and found the maternity register not completed and showed the maternity team what is missing. I gave feedback to the team and the titulaire was there. Two weeks later, when I went back there, I found everything in place. The titulaire despite her busy schedule, took time to fix that herself. You understand that she cares about the work. She did not delegate, she did the work, because she cares.” – ABC mentor |
| Benefits and Drawbacks of Young Leadership | “My impression is that you have a country with a relatively young leadership. Relatively young in the sense of it’s a maturing leadership. On one hand, you have this complexity of an incredibly ambitious Ministry of Health at the highest level of leadership. On the other hand, you have different layers of young leaders, who are dynamic but with lack of managerial and technical experience.” -ABC program coordinator “…Rwanda is a young nation. From its background of genocide and civil war, they had to build everything from scratch. We did a lot of things from 1994, almost miracles. But you understand that we are still learning how to build this country.” – Political Leader, Kirehe |
| Losing Trained Staff as a Key Barrier to Sustainable Improvements | “…There are HC like Rwantonde, Kabuye and Gahara, there are factors behind. Normally there were some key persons at the health center we were used to work together. During mentorship, we were working with everyone, but they are specific people that were driving the improving. Unfortunately, most of these people left. They are no longer at the HC either because of the issue of documents (diplome) or just they left because they found another job.” – ABC mentor “This was an error to build capacity on just one person. This was the case in Kabuye Gahara and in other HC. For other Health centers, you can find nurses who have been working in that department(maternity) for many years, so they bring a new staff, it is a problem because he/she will start from scratch.” – ABC mentor |
| Unplanned Adverse Events Go with Unexpected Great Opportunities to have an Impact on Neonatal Outcomes. | “I think [The change in ANC coverage] makes totally sense (changes in antenatal care coverage). If you look the baseline and during ABC, there was no famine yet or maybe it was not much. But it got worsened in the end of 2015 and 2016 which is the period of sustainability. Maybe the drought started a bit early, but people started to feel it in that period. And it was terrible. I know people who flee the country to Tanzania and Uganda because of the famine.” – Health center nurse “There was a time, there were few pregnant women coming in our health center for antenatal care visit. And when we asked community health workers, they explained that people are very hungry because of the drought. Husbands prefer to flee the country to find jobs. They leave their wives and children home. It is difficult to go to travel to health center when you are hungry and alone at home.” – Nurse from Health center in S. Kayonza “At Kirehe hospital, normally we receive between 150 to 200 of women in maternity per month. But when Burundian refugees came in, we were overwhelmed with pregnant women with more than 300 of admissions per month. Most of the women came from Mahama.” – Nurse at Kirehe hospital |
| Building Self-reliance, Encourages internally Generated Solutions | “In Ndego, the health center worked with CHWs to identify women who missed their appointment- to sensitize them to return to health center for follow-up. They also talk to the women in the village to understand why they don’t return. This has happened in Ruramira too. Even though there were some quality issue but they had a register where they document women who missed their appointment to track them later. They used to call them. This helped a lot to increase the number of women who come for antenatal care visit.” – ABC mentor |
| Gap Between High Demand in Maternal and Neonatal Services and Adequate Human Resources | “If the hospital leadership knew deliveries went up from 200 to 300 in a month because the flux of refugees with only 12 nurses in maternity working day and night for 7 days a week, they should be able to recruit more nurses to adjust. Otherwise, what are you expecting for the 12 nurses to do in front of the increasing demand? Same for neonatology, a lot has been done during intensive phase and mortality went down significantly. There was a time 1 nurse alone had to manage 30 sick babies. Of course, mortality will go high. So, if deliveries went high, the number of sick babies will go high too, and the number of babies with birth asphyxia too. So, I think if the hospital can’t take measures to hire more personnel you understand there is an issue. So here I may say that health providers did not do a good job, but it is not their fault. The problem is they were overwhelmed.”- Health center Nurse in Kirehe |
