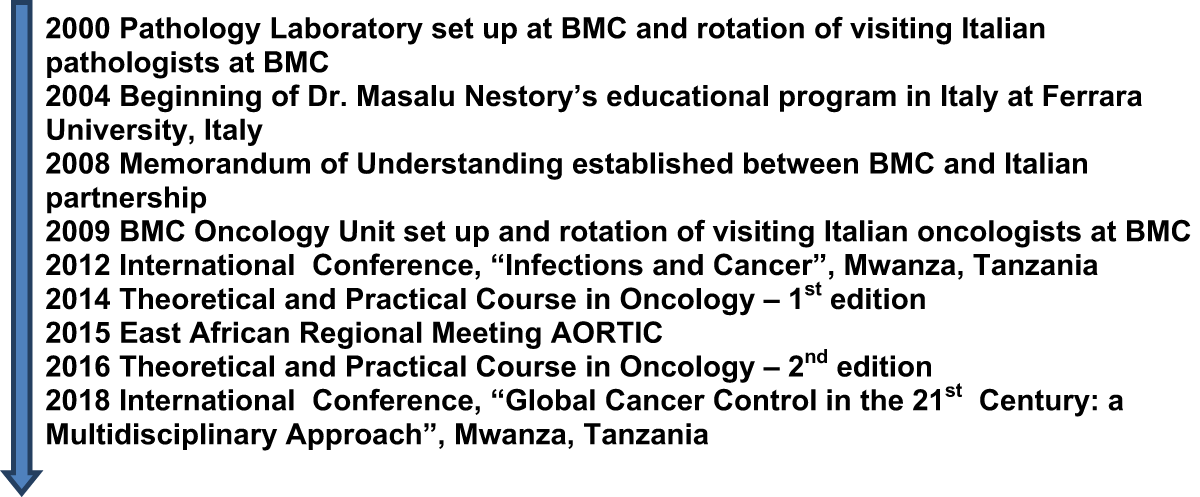
Figure 1
Timeline of the educational program.

Figure 2
Tanzanian nurses preparing chemotherapy (February 2010).
Table 1
Impact of medical education program on Bugando Medical Centre.
| Before medical education program (up to 2015) | After medical education program (after 2015) |
|---|---|
| Improper use of beds (also sometimes used to prepare chemotherapy). | Beds only used for sleeping. |
| Patients chose beds at random each night and beds often shared by more than one patient. | Same beds used for one patient only. |
| Photosensitive drugs not covered. | Photosensitive drugs covered. |
| Incorrect drug administration due to technical errors or to the need for adjusted dose because of poor economic status of patients (drugs paid for by patients). | Correct drug administration. Drugs paid for by Tanzanian government |
| Inadequate chemotherapy preparation (no personal protection, absence of laminar flow hood, inadequate dose preparations and wrong modality of drug dilution, i.e., half dose sometimes administered, needles touched by operators). Unclean surfaces before and after chemotherapy preparation. Same syringe used for multiple preparations. No cups and dresses were available | Carbon filtered masks now used for preparation of chemotherapy. Laminar flow hood acquired. Full chemotherapy doses prepared. Drugs diluted using glucose solution when necessary. Surfaces cleaned with sodium hypochlorite is before and after chemotherapy preparation. Single syringe used for each preparation. Presence of cups and dresses. |
| Drugs prepared and administered in the same room. | Drug preparation occurs in a separate room. |
| Unskilled operators. | Operators trained in procedures to have a correct management of the therapy and patients. Implementation of hand washing procedures. Pharmacists and technicians now present in BMC Medical Oncology Unit. |
| Lack of knowledge about therapeutic schedules relating to different cancer types. | Therapeutic schedules relating to different cancer types provided by IRST. |
| Lack of 250 ml saline solution (solution prepared from bottle of 500 mL saline solution by naked-eye estimation. | 250 mL saline solution now available. |
| Lack of electronic database with patient information (also for toxicity). | Database set up with data inserted on blood tests and clinical pathological characteristics of patients. |

Figure 3
International Conference ‘Global Cancer Control in the 21st Century: a Multidisciplinary Approach’ (Mwanza, 2018).
