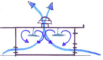
Figure 1
The existing HUM ED. The original ED featured only 15 beds (pink and red above). To expand capacity an observation area with seven beds (blue) and central chairs where patients can be seen were added.
Table 1
Factors to consider when planning ED size. ED patient census is affected by ED throughput (internal factors), determinants that impact arrivals (input factors) and those that impact disposition (output factors). For example, in settings where patient volumes markedly fluctuate by season or time of day, it may be necessary to have areas of the ED that can open and close as needed.
| Input factors | Internal Factors | Output Factors |
|---|---|---|
Demand
| Staff
| Admitting capacity
|
Table 2
Overview of the advantages and limitations of oxygen systems. Options with wall-access are clinically convenient, but require more maintenance, while any choice involving O2 cylinders is laborious and requires mechanisms to refill and replace cylinders. Cylinders may run out without being noticed and may fall over.
| Oxygen System | Wall-accessed | High-flow O2 (15 L/min) | Requires O2 Cylinders | Requires electricity | Requires space at bedside | Capital cost | Operational cost | Maintenance effort | Overall Recommendation |
|---|---|---|---|---|---|---|---|---|---|
| Piped from centralized O2 concentrator | + | + | – | + | – | $$ | $$ | ++++ | **** |
| Piped from a local manifold of O2 cylinders | + | + | + | + | – | $$ | $ | ++ | *** |
| Individual bedside concentrators | – | – | – | + | + | $ | $ | ++ | ** |
| Bedside cylinders | – | + | + | – | + | $ | $ | + | * |
Table 3
Overview of construction and operating costs of different ventilation options. Energy costs are based on HUM ED size and electricity costs in Haiti.
| Ventilation Strategy Options | Description | Construction* | Annual Energy + Maintenance | Projected 10-year cost |
|---|---|---|---|---|
| 1) Passive ventilation |
| $0 | $0 | $0 |
| 2) Improved passive ventilation with elevated roof |
| $32,000 | $0 | $32,000 |
| 3) Mechanical Ventilation |
| $8,500 | $3,750 | $46,000 |
| 4) Air Conditioning |
| $25,000 | $12,000 | $145,000 |
[i] * Costs above baseline of a traditional passive ventilation scheme for an ED the size of HUM based on construction costs in Haiti.
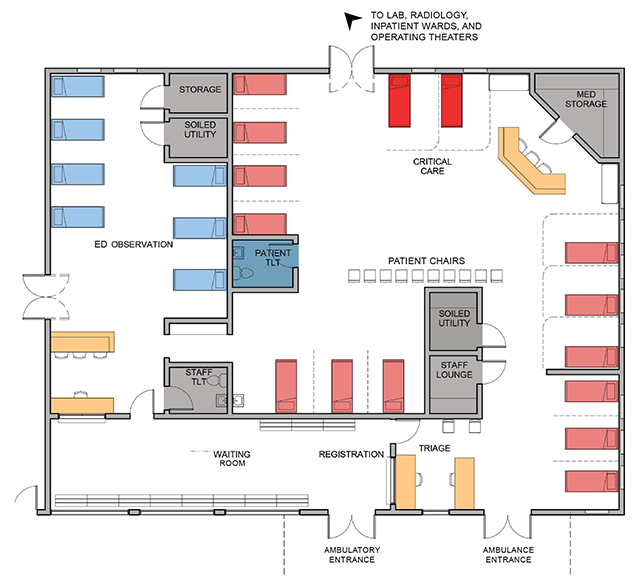
Figure 2
Negative pressure is achieved in an isolation room using mechanical ventilation and unidirectional airflow.
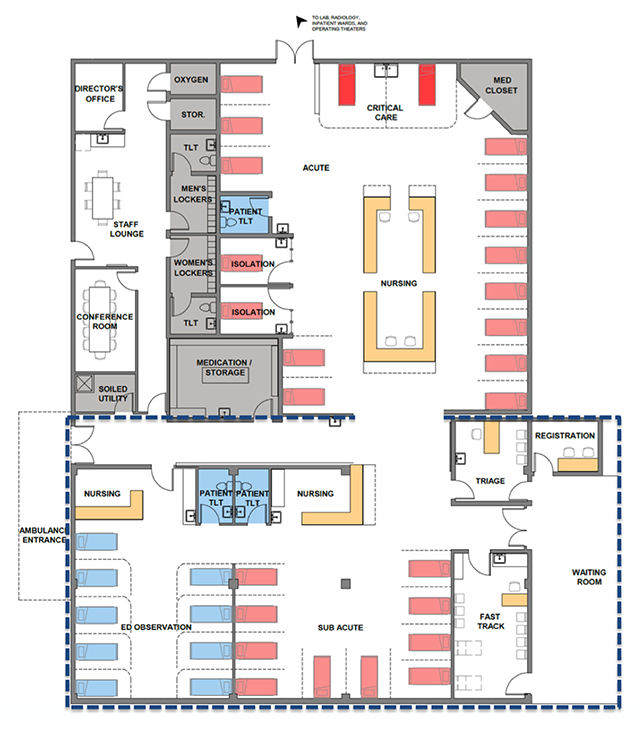
Figure 3
HUM ED Redesign. The dashed box indicates new construction, whereas the remainder of the space reflects redesign within the existing footprint of the HUM ED. Patients move from the waiting area to dedicated triage space into the appropriate fast-track, acute, sub-acute, or observation areas. Staff workspace is positioned to prioritize line-of-site to critical patients.