Sleep is a physiological, periodic and reversible state characterised by partial and temporary suppression of sensory responsiveness and consciousness, while maintaining vegetative functions. It represents an essential biological process responsible for restoring the body’s metabolic and energy balance and ensuring normal neurological activity. Sleep is one of the key features of human biorhythmicity, alternating with wakefulness in a 24-hr nychthemeral cycle. It is an active and complex process rather than a passive one (1). The circadian rhythm, fundamental for maintaining physiological balance, regulates the alternation between wakefulness and sleep. It is controlled by the suprachiasmatic nucleus through melatonin secretion, which increases during the night and decreases with light exposure. Disruption of this rhythm leads to multiple sleep disorders, ranging from insomnia and hypersomnolence to irregular sleep-wake syndromes. Among the most frequent are those related to lifestyle factors such as shift work disorder and jet lag (1, 2). Night-shift work is associated with significant physiological and psychological consequences, including impaired sleep quality, metabolic and cardiovascular dysfunctions and reduced work performance. According to the World Health Organization (WHO) (3) and the International Labour Organization (ILO) (4), irregular work schedules increase the risk of cardiovascular disease, obesity, diabetes, gastrointestinal disorders, depression, anxiety and burnout. The European Directive 2003/88/EC emphasises the importance of rest and recovery time, particularly for personnel engaged in night or rotating shifts.
During the Coronavirus disease 2019 (COVID-19) pandemic, healthcare workers faced unprecedented workloads, continuous exposure to infection risks and emotional strain related to patient outcomes. At the ‘Marius Nasta’ Institute of Pulmonology, the staff experienced sustained physical and psychological pressure, which affected sleep, eating habits and mental health, with potential long-term post-pandemic repercussions (5).
The present study aimed to evaluate the impact of night shifts on sleep quality, fatigue, behavioural and cognitive changes, and perceived stress among medical personnel at the ‘Marius Nasta’ Institute of Pulmonology, comparing the pandemic and post-pandemic periods. Additional objectives included identifying modifiable risk factors, analysing lifestyle habits (smoking, caffeine use, eating behaviour) and assessing the need for psychological support to improve sleep and well-being among night-shift workers.
A descriptive, observational, cross-sectional study was conducted between 9 and 31 March 2023 among healthcare professionals from the ‘Marius Nasta’ Institute of Pulmonology, Bucharest. The research aimed to evaluate the effects of night-shift work on sleep quality, behavioural and cognitive changes and psychological well-being during and after the COVID-19 pandemic (6, 7).
The study included a total of 165 participants, encompassing physicians, nurses, nursing aides and porters.
Inclusion criteria comprised medical or caregiving staff aged >18 years, actively engaged in night shifts, and who voluntarily consented to participate.
Exclusion criteria: refusal to participate, incomplete responses or absence of night-shift activity during the study period.
The final sample reflected the professional composition of the institution with nurses representing the majority of respondents.
Data were collected using a 50-item anonymous questionnaire (Annex 1) designed in Google Forms and distributed via internal communication platforms (WhatsApp groups). The instrument gathered information on demographic and professional characteristics, lifestyle habits, medical history, sleep patterns and perceived stress. The questionnaire combined closed-ended and open-ended questions, allowing both quantitative and qualitative data collection. No identifying information was requested to ensure confidentiality (8).
Collected data included both quantitative (age) and qualitative (gender, work experience, sleep and lifestyle factors) variables. Sleep disturbances, including insomnia, fragmented sleep, daytime sleepiness and nightmares, were identified through self-reported questionnaires in which participants rated the frequency of each symptom (frequently, occasionally, never). These disturbances were not established through medical consultation or psychological testing but were based on participants’ self-perception, following validated self-assessment instruments commonly applied in occupational health research (9, 10).
Lifestyle-related variables included smoking status, caffeine and energy drink consumption, dietary behaviours and exercise habits. Information regarding SevereAcute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) vaccination was also collected without specifying vaccine brands to preserve anonymity.
Data were exported to Microsoft Excel and analysed using IBM SPSS Statistics version 26.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics were expressed as mean ± standard deviation and percentages. Continuous variables were summarised using measures of central tendency (mean, median), while qualitative variables were reported as frequencies and proportions. Differences between dichotomous variables were tested for statistical significance. Graphical representations (figures and tables) were created in Microsoft Excel.
Participants in the study were entirely voluntary and anonymous. All procedures adhered to the ethical principles of the Declaration of Helsinki (2013 revision). Before completing the questionnaire, each participant provided informed consent electronically. The study protocol received approval from the Local Ethical Committee of the ‘Marius Nasta’ Institute of Pulmonology (reference no. 5743/08.03.2023). The confidentiality and anonymity of all collected data were rigorously maintained throughout the research process.
A total of 165 participants were included in the study, of whom 18 (11.3%) were male and 147 (89.1%) female (Figure 1). The participants’ age distribution was as follows: 25–30 years (24 individuals), 30–35 years (32 individuals), 35–45 years (9 individuals), 45–50 years (47 individuals), 50–55 years (40 individuals), 55–60 years (11 individuals) and over 60 years (2 individuals). The 50–55 years age group was the most represented (28.5%) (Figure 2).

Gender distribution of participants.

Age group distribution.
Regarding professional qualification, nurses accounted for 51.5% (n = 85), physicians for 28.5% (n = 47) and nursing aides/caregivers for 20% (n = 33). The majority of participants had been performing night shifts for at least 3 years (Figure 3). The COVID-19 vaccination rate among respondents was high (89%, n = 147), reflecting elevated awareness of occupational infection risks during the pandemic. In terms of lifestyle habits, one-third of participants reported nutritional imbalances such as overeating or appetite loss. Coffee and energy drink consumption was widespread, with 89% of respondents using such products during night shifts.

Duration of night-shift work.
Smoking behaviour showed notable variation. Before the pandemic, 21.8% of smokers consumed between 10 and 20 cigarettes per day; during and after the pandemic, overall tobacco use increased by approximately 50%. Conversely, 14.5% reported quitting smoking, while 10% used alternative nicotine products (e-cigarettes or heated-tobacco devices) and another 10.5% were dual users (Figure 4). Although 34.7% of smokers considered quitting during the pandemic, only 6.7% succeeded, one-fifth of whom did so with professional support through cessation programs.

Increase in cigarette consumption during and after the COVID-19 pandemic. COVID-19, Coronavirus disease 2019.
Chronic conditions were absent in 61.8% of respondents. The most frequent were cardiovascular disorders (17.5%), gastrointestinal (8%) and pulmonary diseases (4.8%). Despite this, only 45% of participants monitored blood pressure monthly, and 40% checked blood glucose annually.
When asked about the impact of night work on daily activities and relationships, 46% reported a significant or very significant effect, while 40% perceived a slight effect. Despite this, 41% still preferred night work, compared to 59% who could opt exclusively for day shifts. The main motivations for accepting night shifts were financial reasons (30%) and availability of time after the shift (26%).
To mitigate fatigue and sleep disturbances, respondents reported adopting various recovery strategies: 37.6% practiced outdoor walking, 24.2% implemented sleep hygiene measures, 18.2% engaged in physical exercise and 16.4% followed balanced diets (Figure 5).

Measures applied to improve sleep quality after night shifts.
Although 96% of respondents considered sleep essential for recovery, 67.9% slept <5 hr during the day following a night shift, while only 4.8% achieved >8 hr of daytime sleep (Figure 6).

Duration of daytime sleep after night shifts.
Before starting the night shift, 15% of participants slept, whereas 37% did not rest at all. OF those who slept, 36% rested <30 min and 7.5% >2 hr. Most participants (94%) stated that daytime sleep was not equivalent to nighttime sleep and 71% did not find it restorative.
Regarding intra-shift recovery, 52.7% believed that short naps of 15–20 min every 2–4 hr would improve performance and alertness (Figure 7).
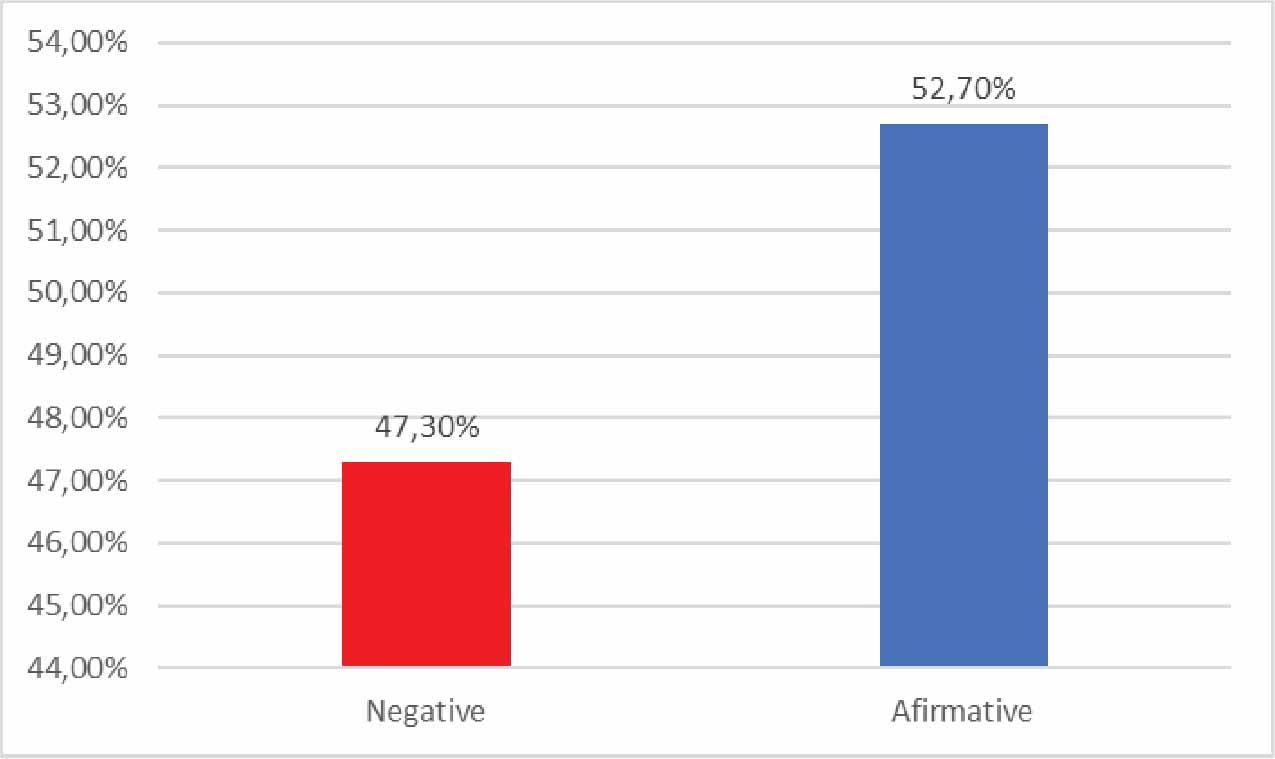
Short rest breaks during night shifts.
The use of hypnotic medication increased from 7.9% before the pandemic to 15.8% after. Sleep deprivation was frequently associated with conflicts in the workplace (31.5%), primarily linked to fatigue and irritability.
Prior to the pandemic, 20.6% of participants reported sleeping <6 hr per night (Figure 8).

Average night-time sleep duration before the pandemic.
The Wilcoxon signed-rank showed a statistically significant difference in wake-up times before and after the pandemic (median 6:00 [5.45–7.00] vs 6.00 [5.00–6.75], P < 0.001), indicating that participants tended to wake approximately 30–40 min earlier after the pandemic (Table 1, Figure 9).

Wake-up time pre/post-pandemic.
Comparison of wake-up time before and after the pandemic
| Parameter | Average ± SD | Median (IQR) | P* |
|---|---|---|---|
| Wake-up-time-ahead (P < 0.001**) | 6.38 ± 1.31 | 6 (5.45–7) | <0.001 |
| Wake-up-time-after (P < 0.001**) | 6.07 ± 1.31 | 6 (5–6.75) | |
| Difference | 0.31 ± 1.01 | 0 (0–0.675) | - |
IQR, Interquartile Range; SD, standard deviation.
Related-samples Wilcoxon signed rank test.
Shapiro–Wilk Test.
Bold values indicate statistically significant results (P < 0.05), as determined by the Wilcoxon signed-rank test.
Conversely, bedtime did not differ significantly between the two periods (median ~23:00, P = 0.732) (Table 2, Figure 10). Self-reported sleep disorders included fragmented sleep (59.4%), insomnia (19.4%), daytime sleepiness (17.6%) and nightmare (3%). Behavioural symptoms reported were nervousness (35.1%), anxiety (30.3%), irritability (23%) and depression (10.9%). Cognitive symptoms included reduced concentration (35.1%), memory impairment (21.2%) and flight of ideas (15.7%) and reduced professional performance (11.5%). Only 15.1% reported no cognitive changes.

Bedtime ante/post-pandemic.
Comparison of bedtime before and after the pandemic
| Parameter | Average ± SD | Median (IQR) | P* |
|---|---|---|---|
| Bed-time-before (P < 0.001**) | 22.75 ± 0.88 | 23 (22–23) | 0.732 |
| Bed-time-after (P < 0.001**) | 22.71 ± 1.02 | 23 (22–23.5) | - |
SD, standard deviation.
Related-samples Wilcoxon signed rank test.
Shapiro–Wilk test.
Regarding psychological impact, 24.9% reported a major impact and 30.9% a minor one. During thepandemic, 24.3% required psychological counselling and 66.7% continued to express a need for such support post-pandemic (Figure 11).

Need for psychological counselling during and after the pandemic.
Finally, 67.2% of respondents reported experiencing persistent stress during day shifts as well, indicating a transfer of night shift-related strain into daytime activity.
This study provides a comprehensive perspective on the multifactorial impact of night-shift work on the physical, psychological and social well-being of healthcare professionals in a post-pandemic context. The findings are consistent with international literature indicating that irregular work schedules and disrupted circadian rhythms significantly influence sleep quality, cognitive function and emotional stability.
The cohort investigated consisted mainly of female nurses aged 45–55 years, a demographic distribution consistent with the structure of the Romanian and European healthcare workforce. Similar patterns have been documented in several studies exploring shift work among nurses in Italy, France and the United Kingdom, confirming that women over 40 years of age represent the majority of personnel engaged in rotating or permanent night shifts (10, 11).
The predominance of women in this professional category is also reflected in the epidemiology of shift-related sleep disorders, where female gender has been associated with a higher prevalence of insomnia and fatigue, potentially due to hormonal fluctuations, dual professional – domestic responsibilities and lower tolerance to circadian misalignment (12). The Alladin study conducted in France (12) found notable prevalence rates of depression (18.9%), anxiety (7.6%), severe insomnia (8.6%) and post-traumatic stress disorder (11.7%) among healthcare workers. In our sample, the rates of insomnia (19.4%), anxiety (30.3%), depression (10.9%) and perceived stress (67.2%) were higher, most likely due to the cumulative burden of pandemic-related stressors. Similar findings have been reported internationally; for example, in Jordan, Yassin et al. (13) identified persistent insomnia in over half of healthcare workers throughout the first pandemic year. Moreover, Hwang and Lee (14) found that depressive symptoms reached 44.3% among intensive care nurses, underscoring the psychological vulnerability of frontline personnel during the COVID-19 pandemic.
Vaccination against SARS-CoV-2 appeared to play a moderating role in perceived stress. In our cohort, 95% of participants had been vaccinated, 49% having received three doses and half reported feeling protected against infection. This aligns with findings showing that vaccine uptake correlates with increased resilience and reduced anxiety among healthcare workers (14).
Night-shift work often prompts maladaptive coping behaviours. Although non-smokers predominated in this study, 63.7% of participants reported increased tobacco consumption following the pandemic, while 89% consumed coffee or energy drinks during night shifts. These trends are consistent with earlier findings linking shift work to stimulant use as a fatigue management strategy (15, 16). However, such behaviours may aggravate circadian misalignment, sleep fragmentation and metabolic dysregulation (17). Furthermore, one third of participants reported dietary imbalance, confirming previous research showing that night disrupts eating habits and may contribute to long-term health declaration (17, 18).
While 96% of respondents acknowledge the importance of sleep for physiological recovery, only 15% slept prior to their night shift and 37% did not rest at all. Similar observations have been reported by Geiger-Brown et al. (19), who found that nurses frequently perceive post-shift sleep as non-restorative. In our study, 94% of respondents stated that daytime sleep was inferior in quality to nocturnal rest, reflecting the persistence of circadian desynchronisation among rotating-shift workers. Despite recognising that work affects general health, participants did not report significant interpersonal conflicts within medical interns, a finding partially consistent with studies highlighting adaptive coping among experienced nurses (20, 21). However, pandemic-related pressures extended into family life: 13.3% of respondents experienced major domestic issues and 20% described occasional tension. Nearly half (49.7%) acknowledged professional difficulties directly associated with the pandemic. These results echo those of Stimpfel et al. (22), who linked extended working hours and night shifts to heightened burnout and reduced job satisfaction.
From a physiological standpoint, night work disrupts circadian rhythms and alters neurobehavioural regulation. The Three-Process Model of Alertness proposed by Åkerstedt and Folkard (23) explains how circadian and homeostatic mechanisms jointly determine sleep latency and performance levels. Disruption of this equilibrium leads to reduced alertness, shortened sleep duration and impaired cognitive control (24–26). In the current study, respondents reported substantial alterations in sleep patterns – nighttime sleep before the pandemic averaged 6–8 hr, while post-pandemic it shortened further with earlier morning awakening (60% by 6 a.m. compared to 49.7% before the pandemic).
These changes were accompanied by a wide spectrum of adverse effects: fragmented sleep (59.4%), nightmares (3%), daytime sleepiness (17.6%) and symptoms of chronic fatigue. Behavioral manifestations included nervousness (35.1%), anxiety (30.3%), irritability (23%) and depression (10.9%). Cognitive outcomes were similarly concerning: reduced concentration (35.1%), memory difficulties (21.2%), flight of ideas (15.7%) and diminished professional performance (11.5%). These findings correspond with international studies demonstrating that sleep deprivation compromises vigilance, executive functioning and clinical decision-making accuracy (27–30). Moreover, poor sleep quality has been shown to exacerbate psychomotor impairment among night-shift nurses (34).
The cumulative impact of night-shift work and pandemic stress generated pronounced psychological effects. Approximately one-quarter (24.9%) of respondents reported a major psychological impact and 30.9% indicated a moderate impact. Such results are consistent with previous research linking occupational fatigue and environmental factors to emotional exhaustion and reduced cognitive efficiency (31, 32). Encouragingly, two-thirds (66.7%) of participants expressed willingness to access psychological counselling and 24.3% had already benefited from such support. This openness to psychological intervention confirms a growing awareness of mental health as an integral component of occupational well-being (17, 32).
Overall, this study reinforces existing evidence that rotating night-shift work – particularly when compounded by pandemic-related stressors – has implications for sleep quality, cognitive functioning and emotional stability. The findings align with earlier analyses emphasising that humans are biologically predisposed to diurnal activity and nocturnal rest and that disruption of this cycle undermines both personal health and professional performance (18, 33).
Given these observations, institutional policies should prioritise the implementation of structured fatigue management programmes, optimisation of shift schedules and systematic psychological support for healthcare professionals. Such interventions can enhance occupational resilience, safeguard patient safety and promote long-term workforce sustainability in post-pandemic healthcare systems.
This study provides evidence of significant disruption in sleep architecture among healthcare professionals working night shifts, particularly in the context of the COVID-19 pandemic. Adherence to evidence-based sleep hygiene principles remains essential to mitigate the physiological and psychological effects of sleep deprivation. Multidisciplinary interventions are imperative for healthcare workers affected by shift-related disorders exacerbated by pandemic-related stress. Integrating professionals such as psychologists, smoking cessation counsellors and lifestyle medicine specialists into occupational health teams can substantially enhance resilience and recovery. The persistence of post-pandemic sequelae appears to depend on multiple interrelated factors, ranging from traditional risk determinants (e.g., smoking, pre-existing cardiovascular disease, insufficient nocturnal sleep) to behavioural contributors such as caffeine overuse and inadequate daytime recovery. Addressing these consequences requires systematic post-pandemic screening, with occupational medicine specialists playing a pivotal role in evaluating cognitive function and psychomotor accuracy through standardised assessments. Finally, this study can serve as a foundation for the development of a coherent national strategy aimed at supporting healthcare professionals who worked night shifts during and after the pandemic. Rehabilitation and recovery programmes designed for this population may yield substantial long-term benefits for both individual well-being and institutional efficiency, as also demonstrated in previous research (18, 33).
This study employed an observational, descriptive, cross-sectional design and therefore cannot establish causal relationships between night-shift exposure and sleep quality. Moreover, as the present research is descriptive and not comparative in nature, it does not allow for inferential statistical analysis or direct comparison between subgroups. The findings should be interpreted as indicative of general tendencies within the studied population rather than as evidence of causal or correlational relationships.
Longitudinal research with repeated measurements is required to differentiate between transient and chronic sleep disturbances. The present findings reflect perceived sleep quality and related disturbances among medical personnel at the ‘Marius Nasta’ Institute of Pneumology during March 2023, without assessing potential long-term or chronic conditions. The sample also displayed a slight gender imbalance – 11.3% male and the remainder female participants – with heterogeneous age distribution, which may have influenced certain outcomes. Nevertheless, this composition accurately reflects the predominantly female structure of the nursing profession and the pneumology specialty. Despite these limitations, the study offers valuable real-world insights into the combined effects of night-shift work and pandemic-related stressors on healthcare professionals.
Future research should focus on three complementary directions. First, comparative studies assessing sleep quality between nurse’s night shifts and other categories of shift workers would clarify the specificity of occupational sleep disturbances. Second, longitudinal observational designs are necessary to monitor temporal patterns in sleep quality, fatigue and psychological well-being, thereby distinguishing between short-term adaptations and chronic outcomes. Third, interventional studies evaluating the effectiveness of strategies aimed at improving sleep hygiene, promoting recovery and optimising workplace ergonomics could generate actionable evidence for institutional policy and workforce health management.
Such research would provide robust data to infirm the design of evidence-based programmes that mitigate the adverse effects of night-shift work and support sustainable occupational health among healthcare professionals.