Acute coronary syndrome (ACS) is a range of medical conditions characterized by abrupt reduction in myocardial blood flow, contributing significantly to global morbidity and mortality rates.1 Recent global data indicate that cardiovascular diseases, including ACS, account for around 3.8 million deaths each year in Europe, highlighting their ongoing role as the leading cause of death both on the continent and globally.2 Moreover, heart conditions have a significant influence on public health and the global economy due to their substantial costs (considering prevention, patient evaluations, hospitalizations, treatment, etc.).3,4
In Romania, the burden is particularly severe, with cardiovascular diseases accounting for a significant proportion of all deaths. Furthermore, the accessibility of current reperfusion procedures is still not adequate.5 These concerning data highlight the urgent need to explore and implement effective prevention and management strategies for ACS, particularly those targeting modifiable risk factors.
The pathophysiology of ACS is complex, involving atherosclerotic plaque rupture, inflammation, thrombosis, and endothelial dysfunction.6 These processes are influenced by a multitude of risk factors, including hypertension, hyperlipidemia, smoking, diabetes, and obesity, many of which are modifiable through lifestyle changes.7,8 Patients with ACSs may have poorer outcomes if other comorbidities are present.9
Nutritional status has emerged as a crucial determinant in the onset and progression of ACS. Malnutrition, characterized by either undernutrition or overnutrition, can exacerbate the inflammatory milieu and oxidative stress associated with coronary artery disease, directly impacting patient outcomes. Recent studies indicate that inadequate nutritional status is not only a risk factor for the onset of ACS but also acts as a standalone prognostic factor in those affected by this disease.10
The impact of nutrition on cardiovascular health goes beyond conventional dietary guidelines aimed at managing lipid levels and blood pressure. Emerging evidence indicates that specific nutritional interventions, such as the Mediterranean diet, high in polyunsaturated fats, antioxidants, and anti-inflammatory compounds, can significantly reduce the risk of ACS and improve clinical outcomes in affected individuals.11 Furthermore, personalized nutritional approaches tailored to individual metabolic profiles and genetic predispositions are gaining attention as potential strategies to optimize patient care.12 However, despite the growing body of evidence supporting the beneficial effects of nutritional interventions, the integration of these strategies into routine clinical practice remains inconsistent.
The aim of the present narrative review was to conduct a critical assessment of the influence of nutritional status, dietary patterns, and targeted nutritional intervention strategies on the management of ACS and inflammation. It highlights the need for comprehensive nutritional status assessment in hospitalized patients, particularly those with cardiovascular conditions, using validated tools.13 The article advocates for a multidisciplinary approach, including dietitians in healthcare teams, to enhance patient outcomes, reduce complications, and improve quality of care through targeted nutritional interventions.
The most successful results were presented in studies based on the Mediterranean, vegetarian, and Dietary Approaches to Stop Hypertension (DASH) diets,14 which have the highest level of proof to mitigate the risk of developing heart conditions and to reduce inflammation.
The Mediterranean diet emphasizes the role of vegetables and fruits, beneficial mono-unsaturated fats such as fish oil and olive oil, seafood, white meat, whole grains, and nuts, as well as limiting the intake of refined sugars and saturated fats of animal origin. Over the years, research has consistently shown that the Mediterranean diet has a protective role against coronary diseases. Its preventive effects are thought to be mediated by beneficial influences on body weight, arteriosclerosis, vascular inflammation, blood pressure, and glycemic regulation, among other factors.15 In 2013, the multicenter Lyon Diet Heart Study was published, in which post-myocardial infarction patients who adopted the Mediterranean diet were followed for a period of 27 months. The results of the study showed a 73% reduction in cardiovascular mortality, as well as in the risk of occurrence of nonfatal myocardial infarction.16
Inflammatory processes are pivotal in the development of endothelial dysfunction and atherosclerosis.17,18 The progression of atheromatous plaques is significantly influenced by inflammatory mediators such as cytokines, adhesion molecules on endothelial cells, and white blood cells. These elements are especially crucial in the early phases of atherosclerosis, as they aid in drawing inflammatory cells from the bloodstream.17,19
Research has shown that the Mediterranean diet may have anti-inflammatory effects that contribute to improved endothelial health. Studies suggest that this diet's positive impact on key atherosclerosis risk factors could be attributed to its anti-inflammatory properties. Improved endothelial function and lower levels of inflammatory markers have been associated with adherence to the Mediterranean diet.17,20,21,22,23
Healthcare professionals should prioritize dietary patterns with robust evidence for cardiovascular benefits. Both the Mediterranean and DASH diets, among others, have been shown to reduce mortality rates related to chronic cardiovascular conditions and overall death rates.24,25,26 The mechanisms behind these benefits are examined through various lenses, including the impact of specific dietary components, psychosocial factors, and different pathophysiological processes such as inflammation, oxidative stress, hypertension, and endothelial and autonomic dysfunction. Diets high in plant-based foods and fish are consistently linked with a decreased risk of cardiovascular diseases.27,28
International guidelines recommend several primary dietary patterns, including the DASH, Mediterranean, and vegetarian diets. A detailed analysis from the PREDIMED study, involving 106 individuals with high cardiovascular risk, investigated the effects of the Mediterranean diet supplemented with extra virgin olive oil or nuts.17,29 This research demonstrated significant benefits, including marked reductions in plasma C-reactive protein (CRP) and soluble vascular cell adhesion molecule-1 (sVCAM-1) levels. After three months, the Mediterranean diet, particularly with olive oil or nuts, was associated with lower IL-6 plasma levels and reduced CD49d expression, a molecule that is present on circulating inflammatory cells.17
Several studies have demonstrated that adherence to the Mediterranean diet, particularly when supplemented with extra virgin olive oil, is effective in reducing the expression of endothelial cell adhesion molecules such as Eselectin, intercellular adhesion molecule-1 (ICAM-1), and VCAM-1 (vascular cell adhesion molecule-1).17,20,22 Similar observations were made by Cortes and Carluccio, who noted decreases in levels of soluble ICAM-1 (sICAM-1), IL-6, E-selectin, and CRP.20,22
Embracing a Mediterranean or predominantly plant-based dietary pattern can be vital in both preventing and managing cardiovascular diseases. Extensive research supports the notion that the Mediterranean diet exerts anti-inflammatory effects by lowering levels of circulating and cellular inflammatory markers, which are pivotal in the development of atherosclerosis—one of the primary risk factors for cardiovascular disease.13
In addition to its anti-inflammatory benefits, the Mediterranean diet is also associated with reduced incidence and improved management of hypertension. Current guidelines from the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH)—based on a range of meta-analyses, randomized controlled trials, observational studies, and systematic reviews—indicate that hypertension can be mitigated and cardiovascular risk reduced through dietary modifications and lifestyle changes.31 Recommended dietary changes include decreasing intake of salt and alcohol while increasing the consumption of a variety of fruits, vegetables, and legumes. Such dietary adjustments have been shown to effectively lower blood pressure. Therefore, an effective dietary strategy for managing hypertension includes a focus on lean fish, low-fat dairy products, fruits, vegetables, whole grains, legumes, and olive oil, while decreasing the intake of saturated fats and red meat.32,33
The DASH diet is another extensively researched dietary pattern known for its health benefits. This diet prioritizes the consumption of seeds, poultry, nuts, beans, whole grains, fish, vegetables, and fruits, while minimizing the intake of red meat, sweets, fats, sodium, added sugars, and salt. Current reports support the hypothesis that the DASH diet is linked to a lower occurrence of cardiovascular disease and promotes optimal blood pressure, with indications of other cardiometabolic benefits in patients with and without diabetes, as well as advantages for patients with hyperuricemia.34 Given that individuals with gout in most cases also have high blood pressure as well as other cardiovascular diseases, the DASH diet is an optimal dietary model for improving all these conditions.35
Nutrition specialists and cardiologists agree that a healthy and balanced diet rich in essential nutrients can beneficially influence heart diseases, having the capability to contribute to both the prevention and improvement of inflammation linked to cardiovascular illnesses.
Food plays a crucial role in human health,36,37,38 acting both as a potential health promoter and a pathogenetic factor. Nutrition is a key element of the healthcare system, as the nutritional status of patients can significantly influence their clinical outcomes and prognosis. Advances in nutritional research have led to the identification of essential nutrients and a deeper understanding of their role in metabolism and health maintenance. Essential nutrients are categorized into six groups: carbohydrates, proteins, fats, minerals, vitamins, and water. Individuals have different nutritional requirements depending on factors such as age, sex, and physical activity. If there are persistent imbalances in the consumption of macronutrients and micronutrients, it can result in malnutrition.
Malnutrition can present acutely, subacutely, or chronically, and it may or may not be accompanied by underlying inflammation.39
The guidelines of the American Society for Parenteral and Enteral Nutrition (ASPEN) advocate for a comprehensive approach to assessing nutritional status among patients admitted to the hospital. This evaluation should include a detailed clinical evaluation (including history and physical examination), anthropometric measurements, diagnostic tests, specific laboratory tests, and dietary assessments.39,40,41,42
Considering the physiological, pathological, and psychosocial factors that affect the nutritional status of individuals is crucial during a thorough nutritional evaluation. It is also important to consider that there is not a single variable or test that will accurately and comprehensively evaluate the nutritional status of an individual. The nutritional screening tools presented in the literature are scientifically validated and are available for use in certain categories of populations.13
It is well known that an altered nutritional status can cause unfavorable effects for an individual's health. Research indicates that individuals with total body protein levels below 80% of what is expected experience higher rates of morbidity. Additionally, unintentional weight loss exceeding 10% has been linked to poorer prognosis and extended hospital stays.43,44
In 2019, a publication regarding the dietary management of hospitalized patients highlighted the importance of individualizing nutritional plans and appropriate support through nutritional risk screening during hospitalization and the subsequent detailed assessment of patients at high risk of malnutrition for a more favorable clinical prognosis.45
In modern medicine, there are many validated multidimensional tools for identifying the impaired nutritional status of hospitalized patients with cardiovascular diseases. These evaluation techniques include several parameters related to nutrition and are based on a scoring system to categorize the severity of malnutrition. However, until now, a clear advantage of one technique over another has not been established. Evaluating the nutritional status of hospitalized patients with cardiovascular conditions involves several extensively studied tools. These include the Subjective Global Assessment (SGA), the Prognostic Nutritional Index (PNI), the Nutritional Risk Screening-2002 (NRS-2002), the Geriatric Nutritional Status Risk Index (GNRI), and the Controlling Nutritional Status (CONUT).
The CONUT score evaluates protein levels, caloric status, and immune response in hospitalized patients, using routine laboratory tests that are readily accessible in clinical practice.46 This assessment comprises three key elements: total cholesterol (which indicates caloric depletion), serum albumin (a marker of protein reserves), and the total lymphocyte count (which reflects immune function impaired by malnutrition).47,48,49
The GNRI provides a comprehensive assessment of both the nutritional and inflammatory conditions in individuals who are 65 years of age or older,50 but recent studies show that the GNRI can also be used in young patients,51 as it is calculated from the value of serum albumin concentration, height, and body weight (ideal).
The PNI serves as an indicator of systemic inflammation and can predict the likelihood of in-hospital death for patients admitted to surgery, cardiology, and cancer wards,52,53 and of long-term mortality (3 years), and reflects immune and nutritional status.53,54,55,56,57,58,59,60,61,62,63 The PNI is calculated using two blood indicators, namely total lymphocyte count and albumin levels.
The evaluation of nutritional status using the SGA involves questioning the patient regarding nutritional problems, weight loss, and the type of diet followed. Additionally, the patients are subjected to a physical examination (subcutaneous tissue loss, muscle loss, edema assessment). Using the SGA, nutritional status is categorized as well nourished (A), mild to moderately malnourished (B), or severely malnourished (C).64
To determine the NRS-2002 score, a body mass index (BMI) that is not within normal limits, weight loss, low food intake, and the presence of a severe disease must be taken into account. If at least one of these elements is present, the final part of the screening consists in the assessment of nutritional parameters and classification of the severity of malnutrition.65,66
Recent data emphasize that the likelihood of malnutrition in hospitalized patients is linked to other diseases, pharmacological treatments, and diagnostic and therapeutic interventions.67,68 Numerous studies have demonstrated the efficiency and effectiveness of preventing malnutrition by screening and evaluating nutritional status during hospitalization, to provide nutritional support and therapy to patients.69,70 Although clinical practice guidelines recommend that nutritional screening be conducted routinely at the time of hospital admission, along with a comprehensive nutritional assessment when needed, actual practice often falls short. Consequently, malnutrition frequently goes unrecognized among hospitalized patients.71 Some of the reasons for the non-identification of malnutrition in Romanian include the absence of a dietician from the multidisciplinary medical team, the lack of medical staff, and the lack of time on the part of the medical staff.
Cardiovascular diseases, with the most frequent manifestation being myocardial infarction, continue to represent the first cause of mortality worldwide. It is well known that general nutritional status influences cardiovascular risk factors. Malnutrition is linked to elevated mortality risk in individuals with cardiovascular illnesses and can result in severe health consequences.
Extensive research has demonstrated that a lack of proper nutrition is linked to an adverse clinical result in patients receiving treatment in hospitals. In acute conditions, the presence of malnutrition can support the increase in cardiovascular mortality by favoring the increase in the patient's state of vulnerability and the appearance of post-myocardial infarction complications, being correlated with a negative clinical prognosis. Studies investigating the inflammatory response post-acute myocardial infarction (AMI) have revealed that adverse clinical outcomes are linked with increased levels of circulating inflammatory markers such as cytokines, adhesion molecules, and chemokines. Furthermore, the involvement of different immune cells and of the complement system has a significant role in the onset, development, and destabilization of at-risk atheromatous plaques.72,73
Among the numerous inflammatory markers studied, CRP has been extensively investigated.74 The broader concept of cardiovascular vulnerability encompasses not only unstable coronary atherosclerotic plaques75,76 but also vulnerable blood and myocardium, collectively defining what is now referred to as the ‘vulnerable patient’.77,78,79,80,83
Altered nutritional status, such as hypoalbuminemia, has been linked to higher rates of all-cause and cardiovascular mortality.80,81 Serum albumin levels are influenced by factors such as synthesis and catabolism rates, extracellular distribution, and exogenous elimination. The interplay between poor nutritional status and systemic inflammation results in decreased albumin synthesis and increased catabolic rates.78,79,81,82 Consequently, a deteriorated nutritional status among patients with cardiovascular diseases can lower serum albumin levels83 and exacerbate systemic inflammation, leading to blood homeostasis disturbances, heightened blood vulnerability, and increased cardiovascular risk.78,79,83
Recent studies have highlighted the protective role of micronutrients against cardiovascular diseases.85,86 While conventional cardiovascular risk factors, including diabetes, chronic heart failure, dyslipidemia, hypertension, and smoking, contribute significantly to cardiovascular disease risk, non-traditional factors like inflammation,87 oxidative stress, and malnutrition also play a role in increasing cardiovascular mortality.88
A study conducted in Romania examined a cohort of 89 patients with AMI to assess the effect of elevated inflammatory status following an AMI on nutritional status, as well as the impact of malnutrition and increased systemic inflammation on their post-AMI evolution.79 The study has shown that patients with poor nutritional status had a high level of inflammation and elevated vulnerability markers, such as a low lymphocyte count and high platelet-tolymphocyte ratio, and that these markers were linked to a prolonged hospital stay and an increased need for hemodynamic support following coronary revascularization. Moreover, patients needing hemodynamic support exhibited notably elevated hs-CRP levels both at admission and on the fifth day of hospitalization. The study has also revealed that although patients with AMI had a BMI indicative of overweight or obesity, approximately 15% were malnourished, which has led to an unfavorable hemodynamic response after revascularization. Similar results were reported by other studies in the literature.79,90,91,92,93,94
Figure 1 presents some of the most widely used nutritional status assessment tools and their clinical relevance in ACS,12,34 while Figure 2 shows the nutritional intervention strategies and their impact on ACS.12,34,95,96,97
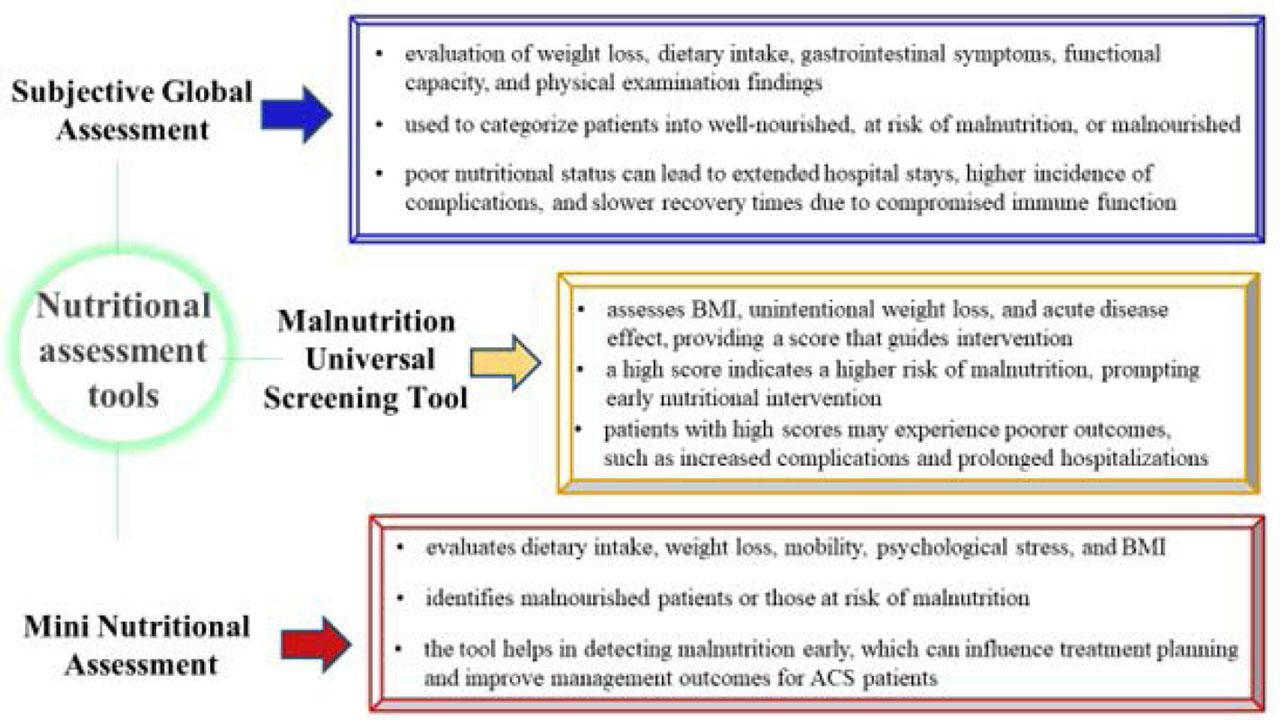
Nutritional status assessment and its clinical relevance in ACS
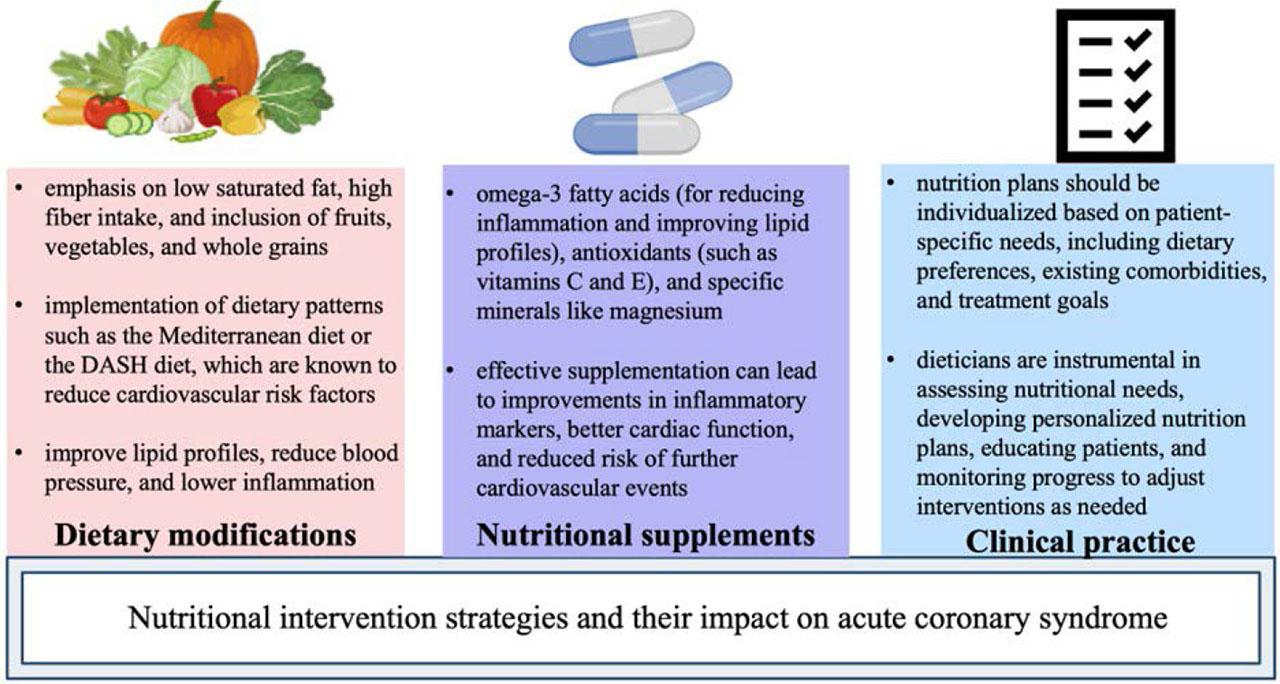
Nutritional intervention strategies and their impact on ACS
Evidence shows that an unbalanced nutritional status negatively affects the health and well-being of patients. To prevent this, significant efforts must be made at several levels of the system (public health, community and individual). Assessing the nutritional state of individuals from the outset, through screening and nutritional evaluation, could enable prompt intervention, decrease the occurrence of complications, and thus facilitate the maintenance of health and a favorable clinical prognosis, enhancing the standard of living for hospitalized patients.
Including a dietitian in the medical team that assesses nutritional status and implements advanced nutritional therapies can help disrupt the vicious cycle between malnutrition and various diseases or acute conditions. A complex nutritional assessment, as well as a systematic nutritional and clinical management based on a multidisciplinary team can reduce the length of hospitalization, recovery time, medical care costs, the risk of complications, and mortality associated with cardiovascular diseases.
Effective collaboration among all members of the healthcare team is crucial for conducting a comprehensive nutritional assessment. As emphasized in this article, the complexity of nutritional evaluation involves multiple components, making it impractical for any single team member to handle these aspects alone. Therefore, physicians, nursing staff, and allied health professionals benefit greatly from working together to ensure the collection of thorough nutrition assessment data. This collaborative approach, which includes integrating a dietitian into the primary care team, enhances patient health outcomes and safety by optimizing the general standard of care.