Glaucoma is one of the most important causes of irreversible blindness in the world due to progressive optic nerve degeneration (1). Based on the state of iridocorneal angle, glaucoma could be classified into two categories: open-angle glaucoma or closed-angle glaucoma. Closed-angle glaucoma has a narrow iridocorneal angle, while open-angle glaucoma is defined by increased resistance in the trabecular meshwork (TM). Both, open-angle glaucoma and closed-angle glaucoma can be primary or secondary. Primary open-angle glaucoma (POAG) is the predominant type of glaucoma (2), while pseudoexfoliation glaucoma (XFG) represents the most important form of secondary glaucoma and is mostly open-angle, but can be also closed-angle glaucoma (3).
POAG is the most highly reported type of glaucoma clinically (4). It is a multifactorial disease in which aging, genetic factors, inflammation and oxidative stress may play a significant role (5).
Pseudoexfoliation syndrome (PEX) is a systemic age-related progressive disorder characterized by abnormal production and aggregation of white extracellular microfibrillar material (6) in multiple organ systems throughout the human body (heart, lungs, kidneys, gallbladder, skin, cerebral meninges, eyes etc.) (7). If PEX deposits accumulate in the anterior segment of the eye, they can obstruct the normal outflow of aqueous humour (AH) causing increased intraocular pressure (IOP) and therefore XFG (8), (9).
PEX may manifest unilaterally or bilaterally. XFG initially develops in one eye before exposed in the other (10). Among the types of glaucoma, XFG has worse prognosis, more damaged visual fiels, a more rapid clinical course, greater optic nerve damage, poorer response to medical treatment and disposes patients to more risk of cataract surgical complications (11).
There are many interactions between thyroid hormones and different diseases. Eyes can also be affected by thyroid gland hormones. This range goes from thyroid-associated orbitopathy (12) to eye changes in hypothyroidism such as conjunctival and periorbital oedema and blepharoptosis (13). This suggests that IOP might be affected by thyroid hormones (14).
However, data regarding connection of thyroid hormones with glaucoma are still poor and inconsistent. Smith's study pointed out that newly diagnosed patients with hypothyroidism had poor outflow of AH, examined with tonography and tonometry (15). After medical treatment of hypothyroidism, AH outflow normalized. Another study didn't find any correlation between IOP and hypothyroidism (16). On the contrary, none of the one hundred patients with hypothyroidism, who had complete ophthalmological examination before and after thyroxine treatment, had been classified as glaucomatous. Lin and others demonstrated a significantly increased risk of open-angle glaucoma development in hypothyroid patients during the 5-year follow-up period, suggesting protective role of levothyroxine (17). Wang and others included 11 studies in their meta-analysis, identifying that hypothyroidism increases risk of POAG development (18). Another study, based on United States population samples, reported lack of connection between hypothyroidism and glaucoma development (19). These contradictory results recommend furthers research of hypothyroidism and glaucoma association.
Thyroid peroxidase is an enzyme that is very important for thyroid hormones' production. Thyroid peroxidase antibodies (TPO-ab) levels increase when immune system falsely attacks and damages thyroid gland cells. These antibodies are found in patients with Hashimoto's thyroiditis and Graves' disease. So far, noone identified significance of TPO-ab in glaucoma disease.
Purpose of this study is to analyze connection between thyroid hormones disbalance and TPO-ab levels in serum with POAG and XFG.
This is a hospital-based retrospective case-control study. The research was performed from June 2023 until December 2023 at Clinic of ophthalmology, University Clinical Center of Kragujevac. The patients were recruited for outdoor department of Clinic for the routine ophthalmological examination from an endocrinologist, with laboratory analysis of serum levels of thyroid hormones and TPO-ab test.
We analyzed serum levels of thyroid stimulation hormone (TSH), free triiodothyronine (fT3), free thyroxine (fT4) and TPO-ab. Based on these results, we divided patients into three groups: POAG patients with hypothyroidism, XFG patients with hypothyroidism and control group that included healthy subjects.
All patients that participated in this study had complete ophthalmological examination: visual acuity test, measured IOP with Goldmann applanation tonometer, biomicroscopic examination of anterior segment, gonioscopy and anterior chamber angle evaluation, as well as fundoscopy. We included patients' gender and age (> 40) as an important data for our study.
POAG patients were defined with presence of retinal nerve fiber layer (RNFL) thinning or defects in visual field followed with IOP levels > 21 mmHg, gonioscopy with the open angle or optic nerve abnormalities (vertical cupping rate > 0.3 cup-disc, asymmetric cupping, peripapillary atrophy etc.) XFG was diagnosed by biomicroscopic examination of characteristic white PEX material over the lens or the iris surface, along with the examination findings counted for POAG. Glaucoma patients, that were included in our study, were using at least one type of anti-glaucoma eye drops.
Blood samples were obtained from the antecubital vein in all patients. The analysis of TSH, fT3, fT4 and TPO-ab levels was performed after the samples stood for 30 minutes in flat tubes and then centrifuged 1500g for 15 minutes. For the diagnosis of hypothyroidism, we used the laboratory reference range for TSH 0.34–5.60 mlU/L, fT3 2.3–4.1 pg/mL and fT4 0.7–1.9 ng/dL. While evaluating TPO-ab, we checked their normal range which should be < 9.0 IU/ml.
IBM SPSS Statistics ver. 22.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis. For comparing TSH, fT3, fT4 and TPO-ab levels among the groups paired t-test and ANOVA were used (p<0.05 and p<0.001 were considered as statistically significant.)
The study included 87 patients who were divided into three groups: POAG group (n=31), XFG group (n=22) and control group (n=34). Sixty-eight were females (76.16%) and nineteen males (21.84%). Highly statistically significant difference among sex distribution was recorded in POAG and XFG group (p>0.001) (Table 1).
Patients' sex distribution
| POAG | XFG | Control | |
|---|---|---|---|
| Female | 23 | 25 | 20 |
| Male | 2 | 3 | 14 |
| Significance | p<0.001 | p<0.001 | p<0.05 |
Mean patients' age in the study was 66.7 ± 6.8 years (median 71, range 42–74 years). The highest mean age was obtained in XFG group (68.4 ± 3.8 years), but without statistically significant difference compared to other groups (p>0.05) (Table 2).
Patients' age distribution
| Groups | n | Mean | Sd | Range |
|---|---|---|---|---|
| POAG | 31 | 66.1 | 4.2 | 44–72 |
| XFG | 22 | 68.4 | 3.8 | 51–74 |
| Control | 34 | 65.7 | 5.2 | 42–70 |
The fT3 and fT4 values were in the range of physiological values in all groups. No statistical significance was seen among the groups in the analysis of fT3 and fT4 values (p>0.05). The highest fT3 value was measured in POAG group (3.6 ± 0.3 pg/mL), then in control group (3.4 ± 0.2 pg/mL), and then in XFG group (3.1 ± 0.4 pg/mL). The highest fT4 was also recorded in POAG group (1.6 ± 0.2 ng/dL), then in XFG group (1.4 ± 0.3 ng/dL), then in the control group (1.1 ± 0.3 ng/dL).
Thyroid stimulating hormone was significantly higher in XFG and POAG groups compared to healthy subjects in control group (p<0.05). Comparing XFG and POAG groups no statistical significance was notices (p>0.05). The highest TSH value was measured in XFG group (7.2 ± 1.4 mlU/L), then in POAG group (5.5 ± 2.5 mlU/L) and then in the control group (1.3 ± 1.1 mlU/L). The same trend was observed in analysis of TPO-ab values. Patients with XFG (60 IU/ml) and POAG (50 IU/ml) had TPO-ab values above the range of physiological values. These results were significantly higher compared to control group (4 IU/ml) (p<0.05) (Figure 1).
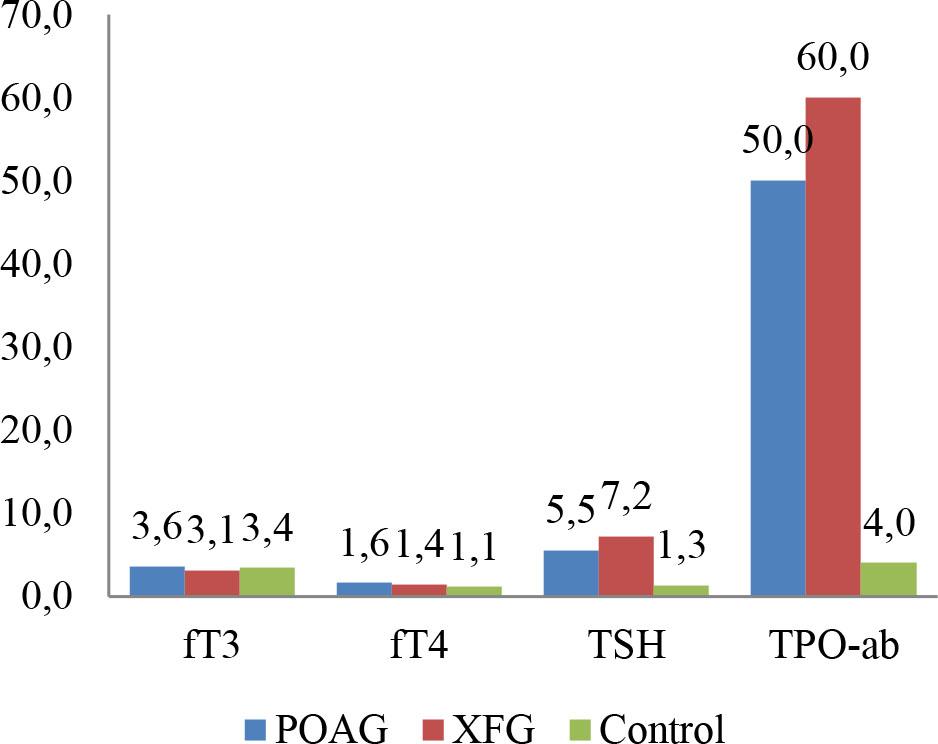
Values of fT3, fT4, TSH and TPO-ab according to the groups
This clinical study demonstrates that there is a statistically significant association between hypothyroidism and glaucoma development. This study is the first of its kind which correlates TPO-ab serum levels and glaucoma development.
Studies that investigate correlation of hypothyroidism and POAG already exist, but there is not enough evidence about possible association between thyroid diseases and XFG (13), (16), (17), (18), (19), (20). Therefore the effect of thyroid hormones' levels in serum on glaucoma development should be more investigated, as well as the potential significant role of TPO-ab.
So far, existing studies include opposed conclusions about the potential connection between thyroid malfunction and glaucoma. Cheng and Perkins reported that among patients with thyroid disfunction, no more than 2% had glaucoma (21). Smith and others found that 23,4% of POAG patients had hypothyroidism (13). They also pointed out a chance that increased IOP could be normalized after treatment of hypothyroidism (15).
It is known that mucopolysaccharides accumulate in dermis and other tissues in patients with hypothyroidism (22). Hyaluronic acid, as a representative mucopolysaccharide and an important part of extracellular matrix, coats the trabecular meshwork, sticking endothelial membranes together (22). Hyaluronic acid accumulates in excessive amount in structures of the eye, creating AH outflow resistance and elevating IOP in hypothyroidism (23). Stein and others found that AH outflow resistance was decreased in 15% of normal eyes and in 48% of POAG eyes after subconjunctival injection of hyaluronidase (24). They suggested that hyaluronic acid takes an important part in the pathogenesis of POAG.
Many studies reveal that patients with PEX material have increased deposition of hyaluronic acid that coats microfibrils of PEX in lens, zonules, iris and ciliary body (25). Also, there are thyroid receptor isoforms on cells of the trabecular meshwork (22). It has been shown that, by bonding with these receptor isoforms, fT3 reduces hyaluronic acid levels. Furthermore, both disorders, hypothyroidism and XFG, have an undesired harmful effect on the vascular endothelium. Those vascular endothelial cells could have a significant role in the ischemia of glaucomatous optic nerve damage (26).
There are studies that suggest that an abnormal immune response to a sensitizing antigen may induce destruction of retinal ganglion cells and the optic nerve (27), (28). Wax and others discovered autoimmune antibodies against heat shock protein 60 in patients with normal-tension glaucoma (29). Later, other authors detected different antibodies in serum of glaucoma patients such as gamma-enolase (30), glutathione-S-transferaze (31), antiphosphatidylserine (32), neuronspecific-enolase (33) etc. This suggests an autoimmune involvement in glaucoma initiation. To support this autoimmune theory, we examined TPO-ab serum levels.
While analyzing fT3 and fT4 serum levels in our glaucoma patients and control subjects, we found no statistical significance among the groups. On the other hand, TSH levels were higher in XFG and POAG groups compared to healthy subjects, which indicates that patients with hypothyroidism have more risk of glaucoma development. Among glaucoma patients, patients with XFG had more increased TSH levels. This supports previous studies that both, patients with hypothyroidism and patients with PEX material, have increased accumulation of hyaluronic acid which creates elevation of IOP.
TPO-ab in control group was in physiological values. Glaucoma patients had increased TPO-ab levels. It is known that the most common cause of hypothyroidism is an autoimmune response, but our results also support autoimmune theory of glaucoma development. It is possible that TPO-ab can be responsible for both, hypothyroidism and glaucoma initiation.
Our study has several limitations. First, 87 patients were included, so future studies should involve more individuals. Also, our hospital-based retrospective case-control study was performed only from June 2023 until December 2023. Prospective longitudinal studies are needed to assess whether or not hypothyroidism is truly a risk factor for glaucoma initiation and progression of disease, analyzing longer period of time. Our glaucoma patients had increased TPO-ab levels, but their potential pathogenic role in glaucoma development should be more investigated.
POAG and XFG have been established to be multifactiorial diseases. They are often the resulf of aging, genetic factors, inflammation and oxidative stress. This study highlights the interaction between thyroid hormones and POAG and XFG development. Patients with hypothyroidism have abnormal accumulation of hyaluronic acid in dermis and other tissues of the human body, as well as in structures of the eye, which leads to increased AH outflow resistance and elevated IOP. Free triiodothyronine reduces hyaluronic acid levels by bonding with thyroid receptor isoforms on TM cells. Previous studies suggest the existence of abnormal immune response which induces the destruction of retinal ganglion cells and the optic nerve in glaucoma. On the other hand, TPO-ab are found in patients with Hashimoto's thyroiditis and Graves' disease. We found that our glaucoma patients had increased TPO-ab values, while healthy subjects in control group had TPO-ab in physiological values. This result supports autoimmune theory of glaucoma development.