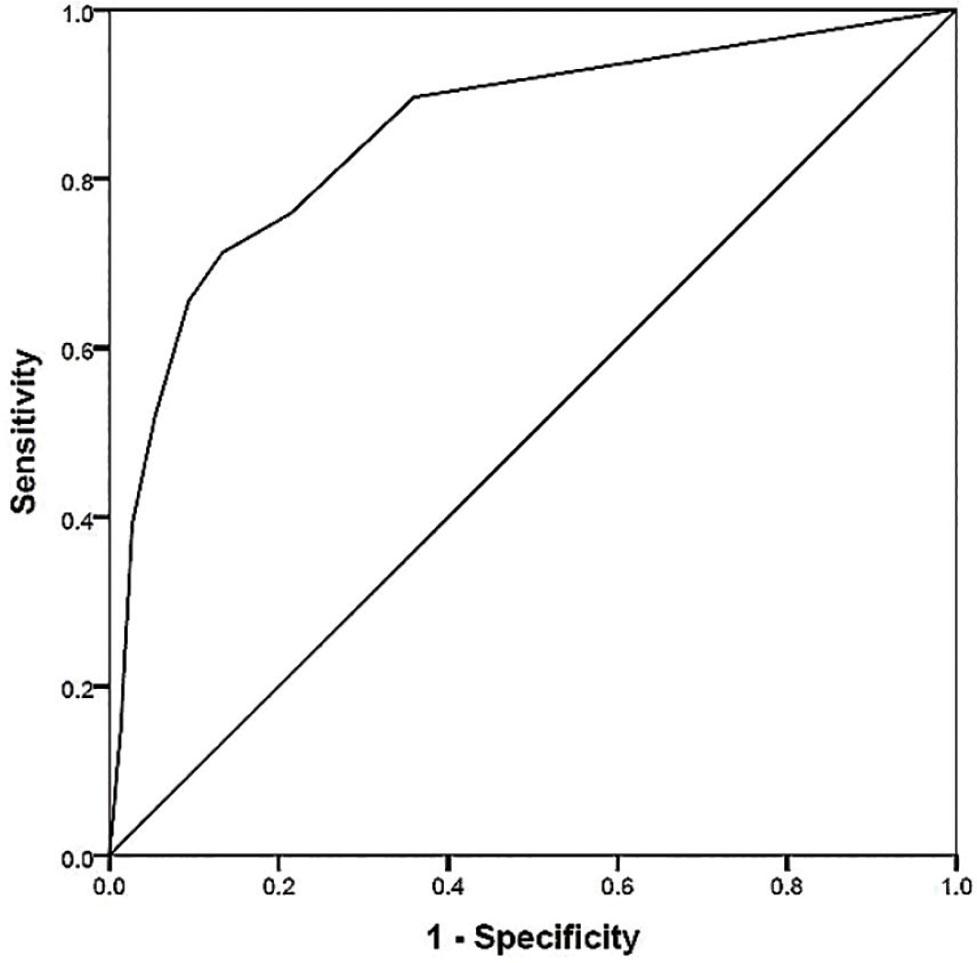
Figure 1.
Multivariate logistic regression of the study population
| Predictors | Univariate analyses | Multivariate analyses | ||
|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |
| Age (years) | 1.035 (1.01–1.06) | 0.02* | 1.03 (0.99–1.08) | 0.16 |
| eGFR | 0.99 (0.97–0.999) | 0.04* | 1.02 (1.00–1.05) | 0.09 |
| New onset of HF or LVSD and suspected CAD | 4.09 (2.02–8.28) | <0.01* | 3.04 (1.23–7.50) | 0.02* |
| Number of leads having STD | 1.59 (1.35–1.87) | <0.01* | 0.77 (0.41–1.42) | 0.40 |
| Summation of leads having STD | 28.74 (8.26–99.97) | <0.01* | 1.99 (0.05–73.80) | 0.71 |
| STE in aVR | 12.32 (4.84–31.36) | <0.01* | 5.56 (1.40–22.16) | 0.02* |
| STE in V1 | 5.60 (2.70–11.65) | <0.01* | 3.48 (1.37–8.88) | 0.01* |
| Anterior STD | 3.47 (0.93–12.96) | 0.06 | 2.32 (0.30–18.28) | 0.42 |
| Lateral STD | 14.67 (6.42–33.53) | <0.01* | 8.41 (1.51–46.88) | 0.02* |
| Inferior STD | 3.21 (1.21–8.54) | 0.02* | 1.05 (0.20–5.63) | 0.96 |
The prediction scores
| Predictors | Point |
|---|---|
| New onset of HF or LVSD and suspected CAD | 1 |
| STE in V1 | 1 |
| STE in aVR | 2 |
| Lateral STD | 3 |
Baseline characteristics of the patients
| Demographic data | All patients (n = 162) | Non-LMCAD/TVD (n = 75) | LMCAD/TVD (n = 87) | P |
|---|---|---|---|---|
| Age (years), Mean ± SD | 66.1 ± 11.5 | 63.7 ± 10.8 | 68.1 ± 11.8 | 0.02* |
| Male sex, n (%) | 91 (56.2) | 43 (57.3) | 48 (55.2) | 0.78 |
| eGFR, Mean ± SD | 72.88 ± 21.98 | 76.68 ± 22.17 | 69.60 ± 21.40 | 0.04* |
| LVEF (%), Mean ± SD | 56.1 ± 16.3 | 59.8 ± 14.3 | 53.0 ± 17.3 | <0.01* |
| New onset of HF or LVSD and suspected CAD | 59 (36.4) | 15 (20.0) | 44 (50.6) | <0.01* |
| Medical history, n (%) | ||||
| Diabetes mellitus | 77 (47.5) | 31 (41.3) | 46 (52.9) | 0.14 |
| Hypertension | 135 (83.3) | 60 (80.0) | 75 (86.2) | 0.29 |
| Dyslipidemia | 135 (83.3) | 61 (81.3) | 74 (85.1) | 0.53 |
| Obesity | 79 (48.8) | 41 (54.7) | 38 (43.7) | 0.16 |
| History of HF | 47 (29.0) | 13 (17.3) | 34 (39.1) | <0.01* |
| Previous MI | 108 (66.7) | 42 (56.0) | 66 (75.9) | <0.01* |
| Prior PCI | 64 (39.5) | 29 (38.7) | 35 (40.2) | 0.84 |
| Prior CABG | 9 (5.6) | 1 (1.3) | 8 (9.2) | 0.04* |
| Peripheral artery disease | 2 (1.2) | 0 (0.0) | 2 (2.3) | 0.50 |
| Previous stroke/TIA | 5 (3.1) | 3 (4.0) | 2 (2.3) | 0.66 |
| Chronic kidney disease | 44 (27.2) | 17 (22.7) | 27 (31.0) | 0.23 |
| Current medication, n (%) | ||||
| Aspirin | 155 (95.7) | 69 (92.0) | 86 (98.9) | 0.05 |
| P2Y12 inhibitors | 120 (74.1) | 51 (68.0) | 69 (79.3) | 0.10 |
| Beta-blocker | 130 (80.2) | 58 (77.3) | 72 (82.8) | 0.39 |
| ACEI/ARB | 105 (64.8) | 51 (68) | 54 (62.1) | 0.43 |
| Non-dihydropyridine CCB | 1 (0.6) | 0 (0.0) | 1 (1.1) | 0.35 |
| Nitrates | 81 (50.0) | 29 (38.7) | 52 (59.8) | <0.01* |
| Statin | 156 (96.3) | 72 (96.0) | 84 (96.6) | 1.00 |
| Mineralocorticoid antagonist | 18 (11.1) | 3 (4.0) | 15 (17.2) | <0.01* |
| Resting ECG, n (%) | ||||
| Number of leads having STD, Mean ± SD | 2.48 ± 2.66 | 1.09 ± 1.80 | 3.68 ± 2.70 | <0.01* |
| Summation of leads having STD (mV), Mean ± SD | 0.37 ± 0.56 | 0.13 ± 0.24 | 0.58 ± 0.66 | <0.01* |
| STE in aVR, n (%) | 51 (31.5) | 6 (8.0) | 45 (51.7) | <0.01* |
| STE in V1, n (%) | 60 (37.0) | 13 (17.3) | 47 (54.0) | <0.01* |
| Anterior STD, n (%) | 14 (8.6) | 3 (4.0) | 11 (12.6) | 0.06 |
| Lateral STD, n (%) | 67 (41.1) | 9 (12.0) | 58 (66.7) | <0.01* |
| Inferior STD, n (%) | 25 (15.4) | 6 (8.0) | 19 (21.8) | <0.01* |