Table 1
Professional background of (A) the steering committee; and (B) of the end-users and experts supporting the steering committee.
| A) MEMBERS STEERING COMMITTEE: PROFESSIONAL BACKGROUND | NO. |
|---|---|
| Orthopaedic surgery (research and clinical) | 2 |
| Neurosurgery (research and clinical) | 1 |
| Physical and Rehabilitation Medicine (clinical) | 1 |
| Physical and Rehabilitation Medicine (research and clinical) | 1 |
| Musculoskeletal physiotherapy (clinical) | 2 |
| Musculoskeletal physiotherapy (research and clinical) | 3 |
| Musculoskeletal physiotherapy (research) | 1 |
| Process management (research and hospital management) | 1 |
| B) SUPPORTING END-USERS AND EXPERTS: PROFESSIONAL BACKGROUND | NO. |
| Musculoskeletal physiotherapy (clinical) | 4 |
| Psychology with expertise in cognitive behavioural therapy (research and clinical) | 2 |
| Psychomotor therapy (clinical) | 2 |
| Occupational therapy (clinical) | 2 |
| Patients | 2 |
| Neurosurgery (research and clinical) | 1 |
| Pathway development (research) | 1 |
| Implementation science (research) | 1 |
| IT and communication department | 2 |
| Clinical support management (clinical) | 1 |
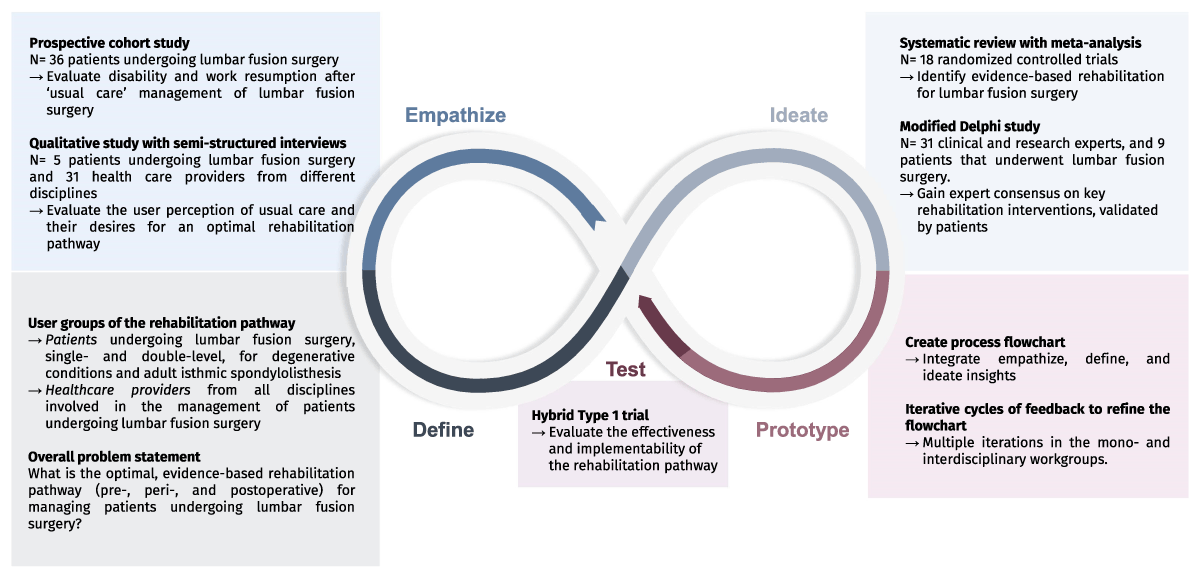
Figure 1
Visual summary of the design thinking infinity loop for developing an integrated rehabilitation pathway for patients undergoing lumbar fusion surgery.
Table 2
Problem statements.
| USER GROUPS | PROBLEM STATEMENT |
|---|---|
| Patients undergoing single- and double level lumbar fusion surgery for degenerative conditions | Patients need tailored rehabilitation in the pre-, peri- and postoperative period, provided by an interdisciplinary team, to improve clinical and work-related outcomes after surgery. |
| Healthcare providers from all disciplines involved in the management of patients undergoing lumbar fusion surgery | Providers need an easy-to-use, evidence-based, interdisciplinary, and transmural pathway to help streamline optimal surgical rehabilitation |
| Overall problem statement: “What is the optimal, evidence-based, rehabilitation pathway (pre- peri and postoperative) for managing patients undergoing lumbar fusion surgery?” | |
Table 3
Outcome indicators to evaluate the effectiveness of the rehabilitation pathway.
| Clinical indicators | |
| Disability (primary outcome) | Oswestry Disability Index |
| Work resumption | Timing and percentage of work resumption |
| Back pain intensity | Numerical Pain Rating Scale |
| Leg pain intensity | Numerical Pain Rating Scale |
| Kinesiophobia | Tampa Scale for Kinesiophobia |
| Depression, anxiety, stress | Depression Anxiety and Stress Scale |
| Pain catastrophizing | Pain Catastrophizing Scale |
| Quality of life | EuroQoL-5D-3L |
| Sit-to-stand performance | Five times Sit-to-stand test (duration) |
| Patient and team indicators | |
| Part of the implementability evaluation | |
| Financial indicators | |
| Direct costs per patient | (1) Inpatient healthcare costs related to the hospitalization for lumbar fusion surgery; (2) Outpatient healthcare costs related to the lumbar fusion surgery; (3) Healthcare costs related to the rehabilitation |
| Indirect societal cost per patient | Sick leave |
| Process indicators | |
| Key rehabilitation interventions | Percentage based on nominator (number of patients receiving the rehabilitation intervention) and denominator (number of patients where the rehabilitation intervention is indicated) |
| Other process indicators | Part of the implementability evaluation |
Table 4
Detailed description of the REACT rehabilitation pathway for patients undergoing lumbar fusion surgery.
| Pathway | The REACT rehabilitation pathway begins with a preoperative intake, and continues up to one year postoperative. The case manager contacts the patient by telephone once the lumbar fusion surgery is scheduled to plan the preoperative intake consultations. Uniform communication of all healthcare providers involved is important. |
| Pre habilitation | Patients receive a preoperative face-to-face intake of 30 minutes with a case manager (preferably with a background in Physical and Rehabilitation Medicine or musculoskeletal physiotherapy), who aims to serve as a contact and trust person during the REACT rehabilitation pathway. All patients receive the same educational leaflet and guidance to a website with educational videos. During the intake session, the content of the leaflet is discussed in a person-tailored manner. This focusses on education (including pain education), setting realistic goals and expectations, creating a therapeutic alliance, promoting a healthy lifestyle including smoking cessation, healthy diet, and psychosocial support. Any potential (biopsychosocial) barriers to the rehabilitation process are also discussed (including a psychosocial screening). Additionally, a 30-minute intake with specialized musculoskeletal physiotherapist, affiliated to the hospital is conducted (including education, teaching postoperative transfers, patient-specific ergonomic advice, encouragement of physical activity). Following these two preoperative intake consultations, the case manager and physiotherapist discuss any points of attention for the rehabilitation (other disciplines can be involved in the interdisciplinary discussion depending on the issues), and the physiotherapist contacts the treating (primary care) physiotherapist to explain the REACT rehabilitation pathway, and essential information for referral. Patients can choose their own physiotherapist. If the patient do not have a preferred physiotherapist, the case manager and specialized physiotherapist may suggest physiotherapists in their local area who are able to align with the philosophy of the REACT pathway. In case of specific issues noticed during the intake consultations, these are addressed, or the patient will be referred for preoperative therapy such as musculoskeletal physiotherapy, psychomotor therapy, psychological therapy or other guidance (e.g. smoking cessation). |
| Peri operative rehabilitation | During hospitalization, early mobilization after lumbar fusion surgery is applied – getting the patient out of bed as soon as possible (no later than 24 hours postoperatively) and avoiding any unsubstantiated movement restrictions. This philosophy of focusing on early mobilization, positive empowerment, and being as liberal as possible regarding movement should be uniformly communicated by all involved healthcare providers and in the educational materials. Patients should receive daily physiotherapy perioperatively (including education, transfers, gait rehabilitation, doing stairs, advice for ADL and participation) that proceeds criteria based. Each patient is discussed interdisciplinary, and other healthcare providers (e.g. psychologist, occupational therapist) can be involved if indicated. Patients receive an X-ray before hospital discharge. |
| Minimal restrictions | Movements and activities with low to moderate axial loading are immediately allowed postoperatively (e.g. bending, rotating, typical household tasks, walking, cycling). Return to work is allowed as soon as feasible. High loading movements and activities (e.g. lifting heavy objects, impact sports) are restricted postoperatively during the first three months. Thereafter, no restrictions do apply. No postoperative bracing is advised. |
| Post operative rehabilitation | Patients continue the rehabilitation with their treating physiotherapist (in primary care). It is advised to start within the first two weeks postoperatively. Physiotherapists will once again be contacted by the specialized physiotherapist (affiliated with the hospital) to provide additional patient-specific information that may have raised during perioperative rehabilitation and to ensure that the physiotherapy aligns with the REACT pathway. Physiotherapists are told that they can always contact the case manager or specialized physiotherapist in case of any questions or concerns that may arise during the initial and further stages of rehabilitation. Physiotherapy includes education, cardiovascular training, functional training of activities (including graded activity), optimization of participation, optimization of posture and movement control (with cognitive behavioral aspects, ergonomic advice, analyzing and treating maladaptive movement patterns, if indicated), and can be discontinued after reaching the goals set by the patient (e.g. specific household task, sport resumption). If indicated (e.g. specific psychosocial risk factors, complicated course), additional healthcare providers can be involved, or an interdisciplinary rehabilitation program affiliated to a hospital can be initiated. |
| Case manager follow-up | Face-to-face follow-up consults with the case manager, lasting approximately 30 minutes, take place at four days postoperatively (or on the last day of a shorter hospitalization) and at six weeks, three months, six months, and one year postoperatively. During these consults, the case manager performs a person-centered history and physical examination, and apply a flexible clinical reasoning approach to evaluate all potential contributing factors to residual symptoms or activity limitations. Additionally, the case manager explores potentially interfering factors with rehabilitation across the biopsychosocial spectrum, and tries to validate potential concerns, provide reassurance regarding the expected course after lumbar fusion surgery and an understandable explanation of residual (or new) pain or symptoms. Medication will be also evaluated, and the rehabilitation plan will be optimized if necessary. Great emphasis should be placed on reassuring and empowering patients to progressively resume their daily activities, sports, and work. Any barriers that patients encounter in doing so should be mapped and addressed. Patients are actively stimulated and supported to resume work. Patients receive the contact information of the case manager (telephone and e-mail), and can contact the case manager if they have questions or concerns. An additional face-to-face consult with the case manager is possible in shared decision with the patient. If a complication or a structural cause of residual or new symptoms is suspected, the case manager will seek additional advice from the treating surgeon. At six weeks postoperatively, patients have a consultation with their treating surgeon. During this consultation, radiographs will be ordered only when clinically indicated. The case manager will oversee the rehabilitation pathway and initiate interdisciplinary discussions when needed. |
