Table 1
Data collection methods across countries.
| CAMBODIA | SLOVENIA | BELGIUM |
|---|---|---|
|
|
|
[i] Note: FGD = focus group discussion, GP = General Practitioner, HT = Hypertension, IDI = in-depth interview, OD = Operational district RN = Registered Nurse, T2D = Type 2 Diabetes.
Table 2
Identified barriers and facilitators to scale-up integrated care, based on the adapted WHO health system building blocks.
| MAIN AND SUB-THEMES | CAMBODIA | SLOVENIA | BELGIUM |
|---|---|---|---|
| 1. Governance | Limited governance for NCDs in line with limited financial commitment from government and donors and low implementation. | Strong centralised governance with strong bureaucracy, with homogeneity across country, although inefficient collaborative governance between levels and sectors for NCDs. | Fragmented, multi-level (partially decentralised) health governance necessitating a multi-stakeholder negotiation model making NCD coordination difficult. |
| 2. Health service delivery | Lack of UHC with low utilisation of public sector for NCD, WHO PEN roll-out is slow. Interprofessional collaboration with nurses/midwives and CHW in PHC. | Near UHC and fairly integrated service delivery due to multi-profile teams and primary care gatekeeping. | Near UHC but variation in primary care practice organisation affecting NCD care. Collaboration in interprofessional teams largely uncommon. |
| 3. Health financing | NCD low budget priority with limited financial coverage, resulting in underpayment of staff in public sector, low public coverage and high OOP. | Relatively modest total healthcare expenditure with a growing share for PHC, with low OOP. Outdated provider payment model demotivates public sector primary care providers with increasing share of private providers. | Inefficiencies in healthcare expenditure across tiers, primary care financing dominated by FFS provider payment system directly impeding IC. |
| 4. HRH | HR capacity insufficient (availability, distribution, skill-mix, due to insufficient mechanisms for motivation, for instance sufficient payment, training in IC provision, leadership and management. Public workforce challenges with moonlighting and brain drain to private sector. | PHC with a relatively good skill-mix and collaboration attitude. Yet GPs are overburdened, dissatisfied, periodically threatening to strike or resign. Policies on task sharing with nurses, initiatives for further task-shifting to lay persons are being tested. | Skill-mix in PHC skewed towards GPs with increasing workload. HRH policies towards IC include new primary care models incentivising multi-professional collaboration and task-sharing, training and organisation to facilitate IC. Differentiated primary care culture across the countries hampering nation-wide roll-out. |
| 5. Medical supply | Overall insufficient availability and logistic systems hampering continuous supply at public facility level, driving people towards private sector. | Well-resourced with access to all modern treatment options for patients. | Well resourced, emphasis on access to newest forms of treatment, with less focus on rationalisation of drug prescribing. |
| 6. HIS | Fragmented and weak, no uniform electronic (web-based) system, no major NCD database. | Fragmented, with no interoperability of different systems. HIS registration by clinicians not prioritised hence of poor quality. | Fragmented, with no interoperability of different systems, notably that of social care with medical care. HIS registration by clinicians not prioritised hence of poor quality, also limited opportunities for population management. |
| 7. Link health system-community | Focus on strengthening role of CHWs and HCWs at HCs. CHWs face challenges relating to technical and financial support, and hierarchy in relation to HCWs. | Focus on low-level care (moving care closer to the patients and their home) and task delegation (towards more emphasis on peer support). | Focus on strengthening linking PHC and social sector (difficult due to varying incentive systems in medical and social sector, e.g. FFS vs. salary) and increasing patient, social worker and local government representation and their roles in coordination of PHC. |
[i] Note: CHW = community health worker, GP = general practitioner, FFS = fee-for-service, HC = health centre, HCWs = healthcare workers, HIS = health information system, HRH = human resources for health, IC = integrated care, MoH = Ministry of Health, NCD(s) = non-communicable disease(s), OOP = Out-of-pocket expenditure, PEN = Package of Essential NCD interventions (implemented in Cambodia), PHC = primary healthcare, UHC = universal health coverage, WHO = World Health Organisation.
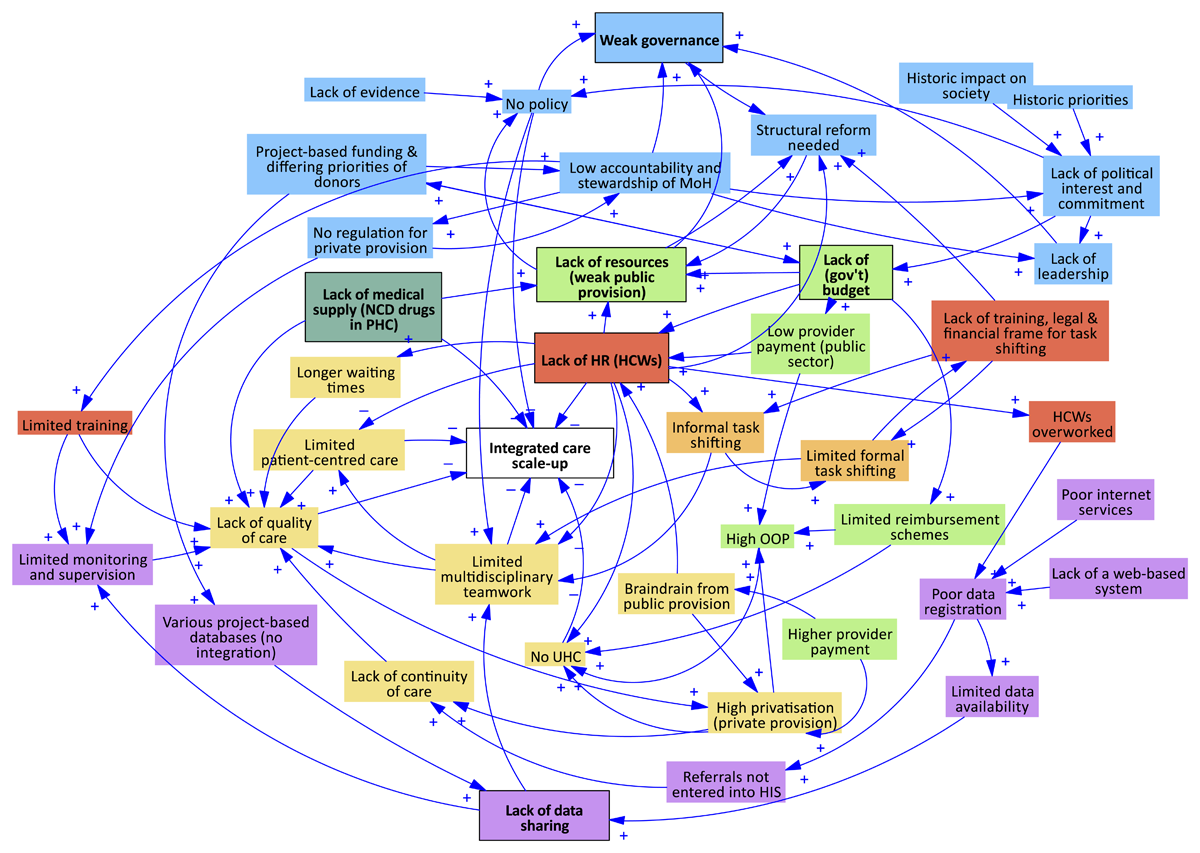
Figure 1
Interactions between health system barriers and facilitators to integrated care in Cambodia.
Note: blue = governance; yellow = healthcare delivery; green = financing; red = HRH; dark green = medical supply; purple = HIS; orange = community.
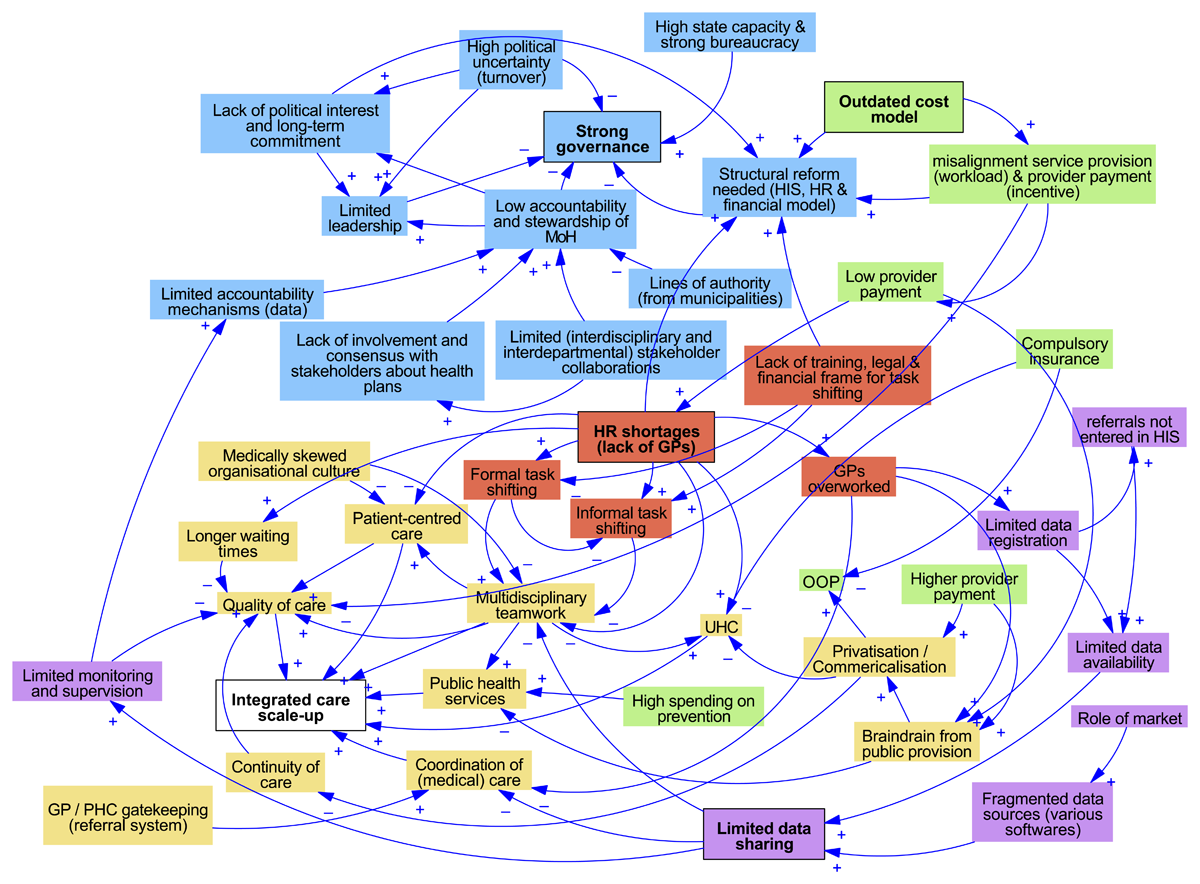
Figure 2
Interactions between health system barriers and facilitators to integrated care in Slovenia.
Note: blue = governance; yellow = healthcare delivery; green = financing; red = HRH; dark green = medical supply; purple = HIS.

Figure 3
Interactions between health system barriers and facilitators to integrated care in Belgium.
Note: blue = governance; yellow = healthcare delivery; green = financing; red = HRH; dark green = medical supply; purple = HIS.
| BoD | Burden of disease |
| CHC | Community health centre |
| CHW | Community health worker |
| CLD | Causal loop diagram |
| FFS | Fee-for-service |
| GDP | Gross Domestic Product |
| GP | General practitioner |
| HC | Health Centre |
| HCW | Healthcare worker |
| HEC | health education centre |
| HIS | Health information system |
| HRH | Human resources for health |
| HT | Hypertension |
| IC | Integrated care |
| ICCC | Innovative care for chronic conditions |
| MoH | Ministry of Health |
| NCD | Non-communicable disease |
| NIHDI | National Institute of Health and Disability Insurance |
| NGO | Non-governmental organisations |
| OD | Operational district |
| OOP | Out-of-pocket expenditure |
| PHC | Primary Healthcare |
| PCZ | Primary Care Zone |
| PEN | Package of essential NCD interventions |
| PESTEL | Political-Economic-Socio-cultural-Technological-Ecological-Legal (factors) |
| PHC | Primary healthcare |
| RH | Referral hospital |
| RN | Registered nurse |
| SCUBY | ‘SCale-Up diaBetes and hYpertension care’ project (website: scuby.eu) |
| T2D | Type 2 Diabetes |
| THE | Total health expenditure |
| UHC | Universal health coverage |
| WHO | World Health Organization |
