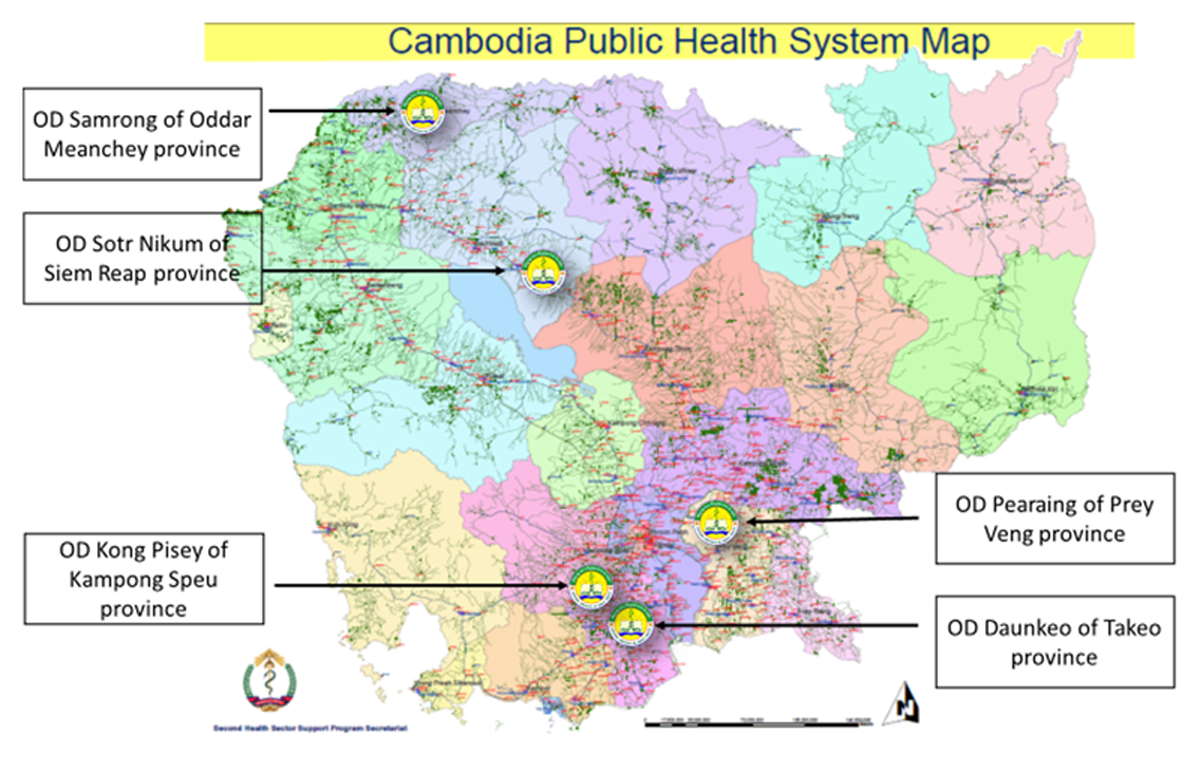
Figure 1
Locations of the five selected ODs in Cambodia.
Table 1
Five ODs and the availability of care initiatives for T2D.
| OD | PROVINCE | COMBINATION OF CARE INITIATIVES | EXISTING CARE PROVISION |
|---|---|---|---|
| 1) Daunkeo | Takeo | Co-existence of the three care initiatives | NCD clinic + WHO PEN + Peer Educator Network |
| 2) Pearaing | Prey Veng | Health centre-based care | NCD clinic + WHO PEN (high coverage) |
| 3) Sotr Nikum | Siem Reap | Health centre-based care with context | NCD clinic + WHO PEN (low coverage) |
| 4) Kong Pisey | Kampong Speu | Community-based care | Peer Educator Network |
| 5) Samrong | Oddar Meanchey | Hospital-based care | NCD clinic |
Table 2
Questions of each ICP component in the grid.
| ICP COMPONENTS | QUESTIONS/ITEMS |
|---|---|
| Component 1: Facility-based identification of patients with T2D | 1.1. To what extent, is screening for T2D performed among patients at a visit? 1.2. To what extent, are equipment and materials necessary for diagnosing patients for T2D available at the facility? 1.3. To what extent, are health care staff or service providers competent to perform diagnosis for T2D at the facility? 1.4. To what extent, is the follow-up of the patients after the screening, testing and diagnosis of T2D organised? |
| Component 2: Treatment of T2D by primary care providers using standardised protocols | 2.1. To what extent, are written guidelines of care and treatment accessible to primary care providers for T2D? 2.2. To what extent, are primary care providers in charge competent to provide treatment for patients with T2D? 2.3. To what extent, are the essential medications for T2D available in the primary care setting? 2.4. To what extent, do primary care providers have necessary laboratory access? 2.5. To what extent, have primary care providers received training for treating T2D? 2.6. How comprehensive is treatment beyond medication prescription for T2D (including measuring of body mass index, waist circumference, blood pressure, cholesterol level, renal function, screening for complications – foot examination, eye problem, macrovascular disease, depression)? 2.7. To what extent, are medication reviews undertaken in the elderly with T2D in order to avoid polypharmacy, hypoglycemia and renal dysfunction? |
| Component 3: Health education and counselling to patients with T2D by non-physician care providers | 3.1. To what extent, do patients with T2D receive information on how to reduce health risks by non-physicians? 3.2. To what extent, are patients informed about the chronic condition of T2D by non-physicians (including the expected course, expected complications, and effective strategies to prevent complications and manage symptoms)? 3.3. To what extent, are non-physicians trained to provide health education and counselling to patients with T2D? 3.4. To what extent, are health education or counselling materials accessible to non-physicians for T2D? |
| Component 4: Self-management support to patients and their informed caregivers with tools for adherence and monitoring | 4.1. To what extent, are patients offered self-management training for T2D (for example, to improve adherence to medications, proper nutrition, having self-monitoring tools at home, consistent exercise, tobacco cessation, and maintain other healthy behaviours)? 4.2. To what extent, do health care staff or community health workers support patients’ self-management efforts on a continuous basis for T2D? 4.3. To what extent, are health care staff or community health workers competent to perform self-management training? 4.4. To what extent, does the patient have access to materials for self-monitoring for T2D, for instance, glucose meter/glucose test strips? 4.5. To what extent, are informal caregivers/non-medical involved in the self-management process for T2D? 4.6. Are the concerns of patients and families addressed? 4.7. Are patient treatment plans agreed with patients, reviewed and written down? |
| Component 5: Structured collaboration between health care workers, community actors, and patients and caregivers | 5.1. To what extent, is there an identified “care coordinator” who serves as the overseer and director of a patient’s care, ensuring that efforts of all involved health care workers, community actors, and patients and caregivers are integrated and coordinated for T2D? 5.2. To what extent, do the health care organisation and the community have complementary functions, that is, the community organisation fills gaps in services that are not provided in formal health care for T2D? 5.3. To what extent, are referral practices systematically organised for T2D? 5.4. To what extent, does cooperation between health care workers and other professionals and community actors occur for T2D? 5.5. To what extent, is the traditional hierarchy flattened and moved away from physician-dominated models for T2D? |
| Component 6: Organisation of care, delivery system design and clinical information systems | 6.1. To what extent, are ongoing quality improvement routine activities among health care workers organised? 6.2. To what extent, do information systems gather and organise data about epidemiology, treatment, and health care outcomes? 6.3. To what extent, do information systems serve as a reminder function for patient specific prevention and follow-up services (e.g. to identify patients’ needs, follow-up and plan care, monitor responses to treatment, and assess health outcomes)? 6.4. To what extent, is feedback about the performance provided to the team and its members? 6.5. To what extent, is an appointment system with planned visits used? |
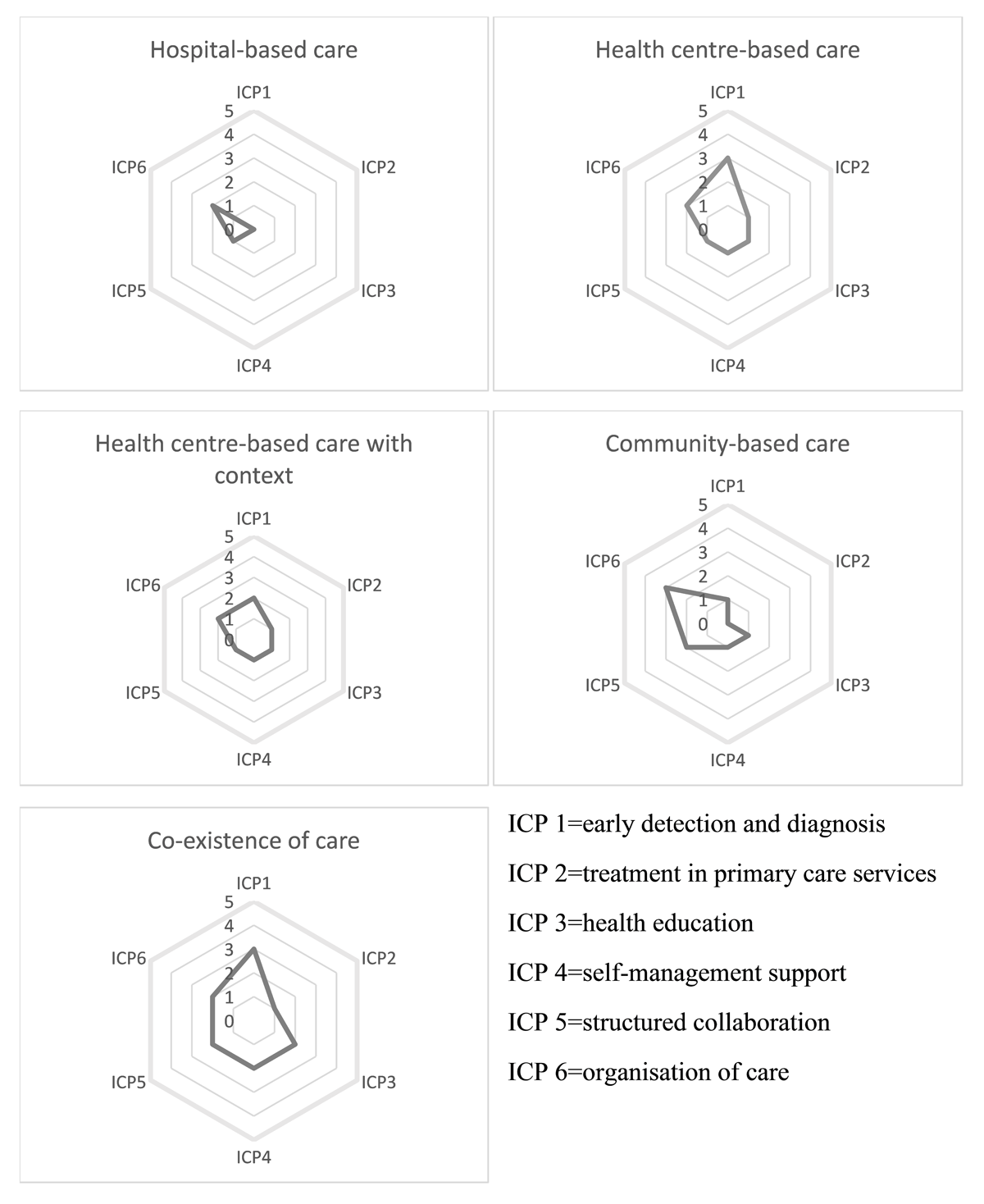
Figure 2
Spider chart representing the ICP components of the care initiatives either individually or in co-existence.
