Table 1
Overview of included Flemish interprofessional initiatives for older people with polypharmacy in primary healthcare.
| INITIATIVE | SETTING | DESCRIPTION | ROLE OF INCLUDED HEALTHCARE PROFESSIONALS |
|---|---|---|---|
| 1 | Ambulatory healthcare | Therapy adherence screener, medication review | The nurse or pharmacist evaluated the patient’s therapy adherence by using a therapy adherence screener to guide the conversation with the patient. Next, the completed screener and the medication schedule were provided to the general practitioner (GP) and pharmacist. The GP and pharmacist conducted a medication review together. Patient education was then provided by the pharmacist, GP or nurse. |
| 2 | Ambulatory healthcare | Proactive monitoring of (poly)medication | The nurse had a conversation with patient to monitor the medication use. Areas of concern were discussed with the GP, who provided a follow-up meeting with the patient. |
| 3 | Ambulatory healthcare | Individual medication preparation, medication review | The nurse had a conversation with patient to monitor the medication use and identified patient who would benefit from individual medication preparation. The GP and pharmacist conducted a medication review together. The pharmacist then conducted the individual medication preparation at the community pharmacy. |
| 4 | Ambulatory healthcare | Multidisciplinary ‘neighbourhood teams’ | The nurse, pharmacist, GP, physiotherapist and psychologist, who work in the same area, had interprofessional meetings to make agreements to optimise pharmaceutical care for specific patient populations (e.g. patients with heart failure). |
| 5 | Ambulatory healthcare | Individual medication preparation, medication review | The nurse or pharmacist evaluated the patient’s medication use. The GP and pharmacist conducted a medication review together. The pharmacist then conducted the individual medication preparation at the community pharmacy and provided patient education. |
| 6 | Nursing home | Interprofessional case conferences | A structured interprofessional case conferences was organised (twice a year) with the nurse, pharmacist, GP and coordinating physician to discuss residents’ medication schedules |
| 7 | Nursing home | Interprofessional case conferences | A structured interprofessional case conferences was organised (thrice a month) with the nurse, pharmacist, GP, coordinating physician, occupational therapist and physiotherapist to discuss residents’ medication schedules. The medication review was prepared by the pharmacist before the case conference. |
| 8 | Nursing home | Interprofessional case conferences | A structured interprofessional case conferences was organised (once in three weeks) with the nurse, general practitioner, nurse aid, occupational therapist, physiotherapist and nursing home director to discuss residents’ medication schedules. |
| 9 | Nursing home | Periodic evaluation of psychotropic drug use | A structured interprofessional meeting was organised (thrice a year) with the nurse, pharmacist, general practitioner, coordinating physician, psychologist and nurse aid. This meeting was prepared by the psychologist who monitored psychotropic drug use and medical records of residents. |
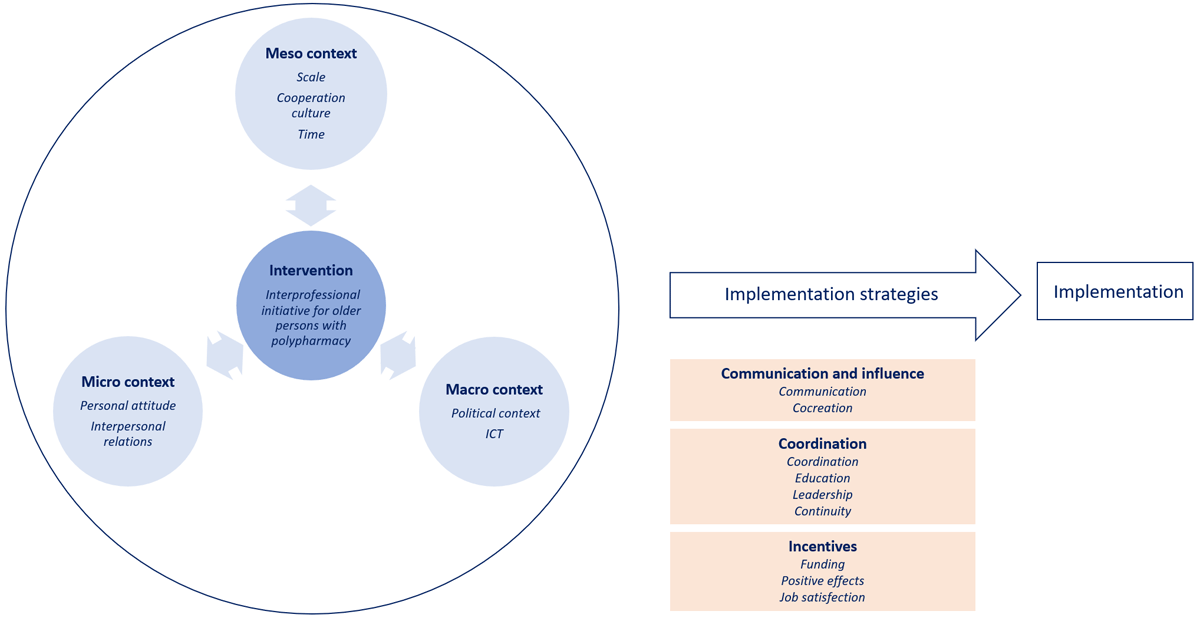
Figure 1
Themes and subthemes influencing implementation of interprofessional initiatives for older people with polypharmacy positioned under the three core elements – intended change (dark blue), context (light blue) and implementation strategies (orange) – of implementation frameworks
Table 2
Quotes illustrating different subthemes related to context factors.
| SUBTHEME | QUOTE | INTERVIEWEE | INITIATIVE |
|---|---|---|---|
| Personal characteristics | In the beginning there was some resistance of our nurses to hand over the task of medication preparation. Or it could be fear to no longer being fully up-to-date. | Nurse | 3 |
| Interpersonal relations | Now they simply know us and our capacities better. There is respect and awareness that we do have medication knowledge. Without IC, this would not be clear. | Pharmacist | 7 |
| Culture of cooperation and intervision | “It should be interprofessional and so they should all be under the same roof”, this is nonsense. There should be a collaborative culture, you should sit together but it is not necessary to work under one roof. | General practitioner | 7 |
| Time creates opportunities | The pharmacists, we collaborate with, are often small scaled pharmacists, who have no time to invest in such collaboration initiatives about polypharmacy. This should be supported much better. | Nurse | 2 |
| Political context | If you were to aggregate the profit of this initiative, it should actually be mandatory. (…) As a GP, you should take it for granted that someone is double-checking your prescriptions. It is so obvious. | Nursing home director | 6 |
| Restricted ICT possibilities | I think the integration of the medical electronic record and the nursing electronic record is a priority to be able to avoid misunderstandings and interactions between medication in particular. (…) It would not solve all the problems but it would make it a lot easier in terms of communication between the different actors in the nursing home. | Coordinating physician | 7 |
Table 3
Quotes illustrating subthemes related to implementation strategies.
| SUBTHEME | QUOTE | INTERVIEWEE | INITIATIVE |
|---|---|---|---|
| Communication | We made a very simple flow chart for three medication classes: benzodiazepines, antidepressants and antipsychotics, presented on a poster visible for the entire staff (…) I think this is very important: translating the evidence into everyday language and no bombastic messages but that everyone could understand and apply it. | Geriatrician | 9 |
| Co-creation | The inspiration (for the initiative) came from within the organisation. Problems were reported, e.g. difficulties with finding information about medication or to give feedback. We saw that there was too little contact with pharmacists about medication use. Hence, we wanted to set up this collaboration. | Nurse | 3 |
| Coordination | It is a multi-year journey and there are still things that need to be improved. (…) It is important to realise that starting up a multidisciplinary neighbourhood team like this, you have to approach it very phased and carefully, don’t want to do everything at once. That won’t work. | Project coordinator | 4 |
| Education | You have to inform and educate all the staff of the nursing home about the different aspects of the medication use. (…) it is very important to get all noses in the same direction. | Geriatrician | 9 |
| Leadership | Giving leadership to HCPs is incredibly important. (…) That makes it for me and my colleagues, the coordinators, a lot easier. We don’t have ‘to pull’ all the time because there’s so much happening bottom-up. | Project coordinator | 4 |
| Continuity | You need a fixed point of contact (of the delivering pharmacy) for the continuity of care. It is important to have trust in each other for the sustainability of the interprofessional consultations. What helps is the fact that you work together for a long time. | Coordinating physician | 7 |
| Funding | Our intention is that hopefully this (initiative) can become something structural and that a nomenclature code can be linked to it in such a way that this becomes the regular operation of the pharmacist. | Project coordinator | 5 |
| Positive effects | We think this collaboration is very important. As nurses, we look at things differently than doctors. They look from the medical and we rather from the practical side. We notice different things. Bringing those two stories together makes it much easier to follow-up someone. | Nurse | 2 |
| Increased job satisfaction | I think everyone feels more appreciated. We work together with respect for each other and for each discipline. I would be very frustrated if I had to do my job without being able to collaborate, and if we would work on separate islands. I would be less motivated to work. So I think that (initiative) stops or removes a lot of internal frustrations. | Physiotherapist | 8 |
