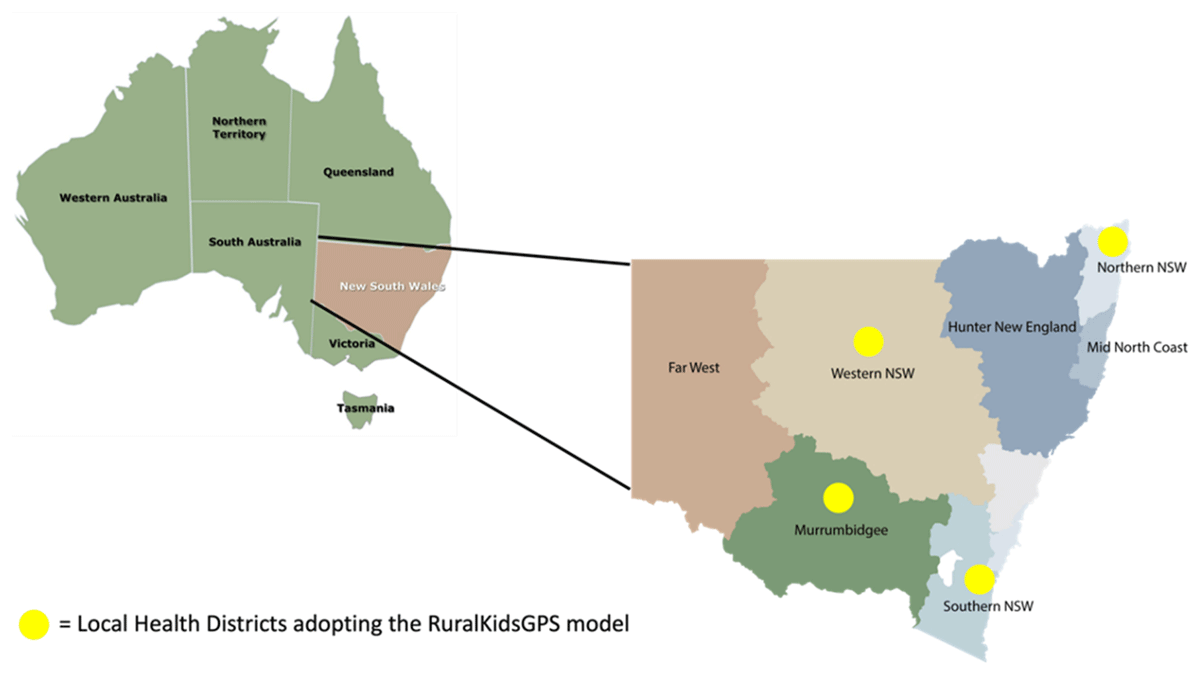
Figure 1
Local Health Districts involved in the RuralKidsGPS study.
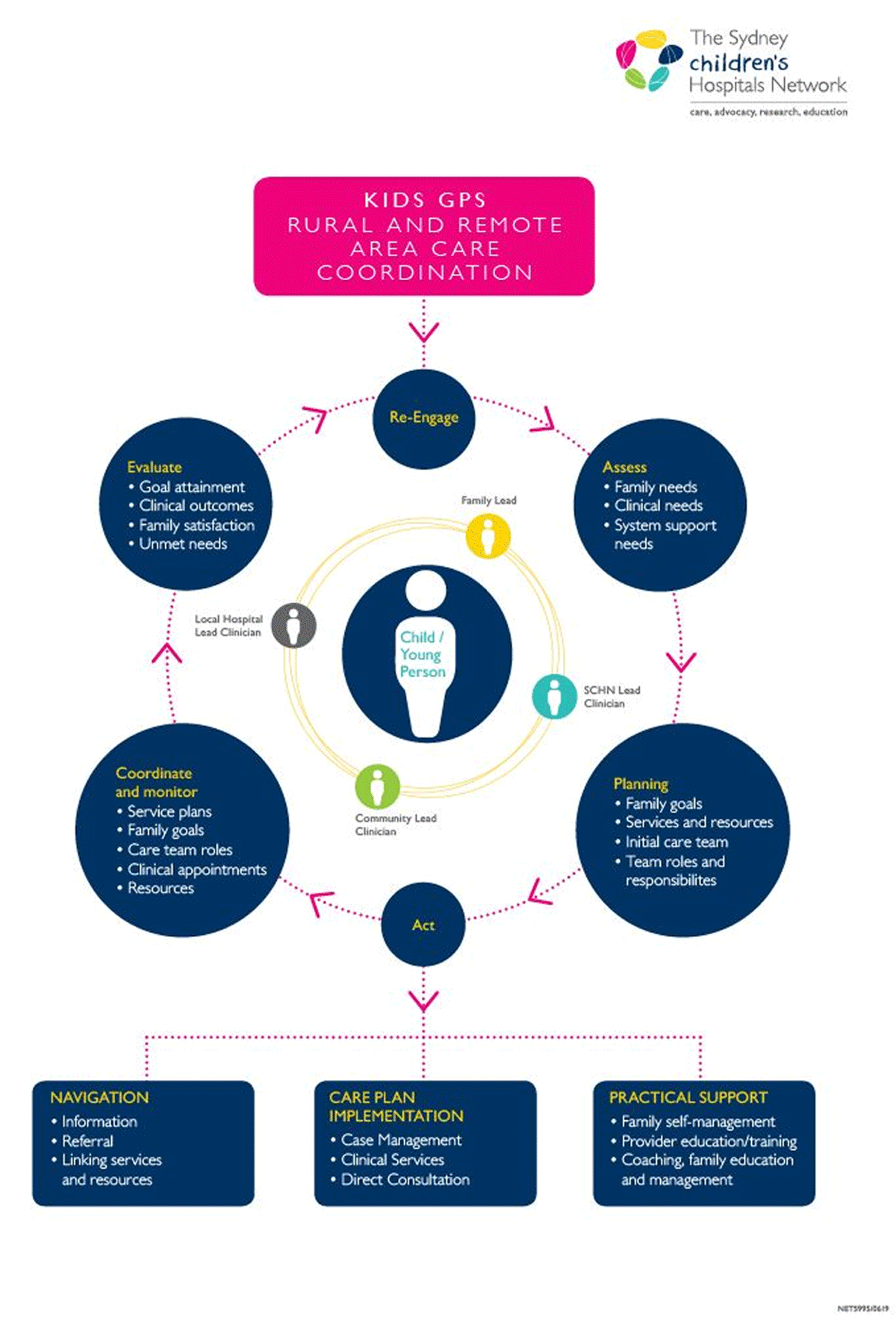
Figure 2
RuralKidsGPS Circle of Coordination (adapted from Cohen, et al. 2011).
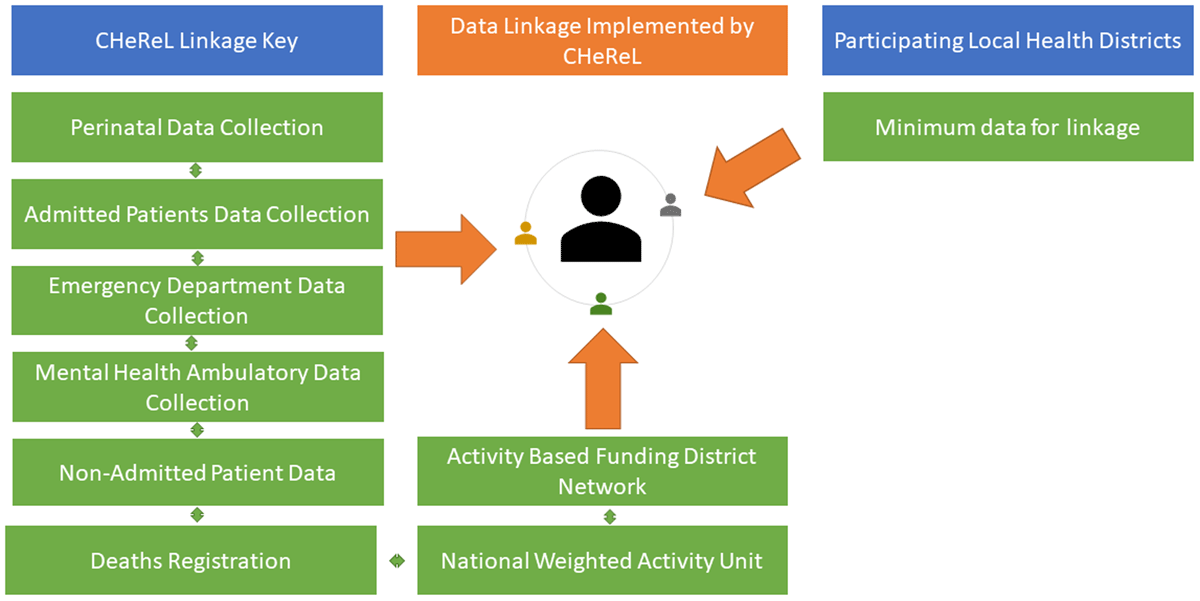
Figure 3
Sources of data for linkage.
Table 1
Family reported outcome measures.
| OUTCOME MEASURES | PURPOSE |
|---|---|
| Paediatric Integrated Care Survey (PICS) [6] | Measures experiences of integration of child’s care |
| Adapted Mumford scale [7] | Measuring non-medical out of pocket expenses for families |
| EuroQol 5 Dimension 5 Level (EQ-5D-5L) [8] | Health status measure |
| Paediatric Quality of Life Measure (PedsQL4.0) [9] | Measuring health paediatric health outcomes |
| Child Health Utility 9D (CHU 9D) [10] | Instrument used to adjust quality of life years from PedsQL4.0 score for economic evaluation |
| Warwick-Edinburgh Mental Well-being Scale (WEMWBS) [11] | Understanding and measuring mental health and wellbeing |
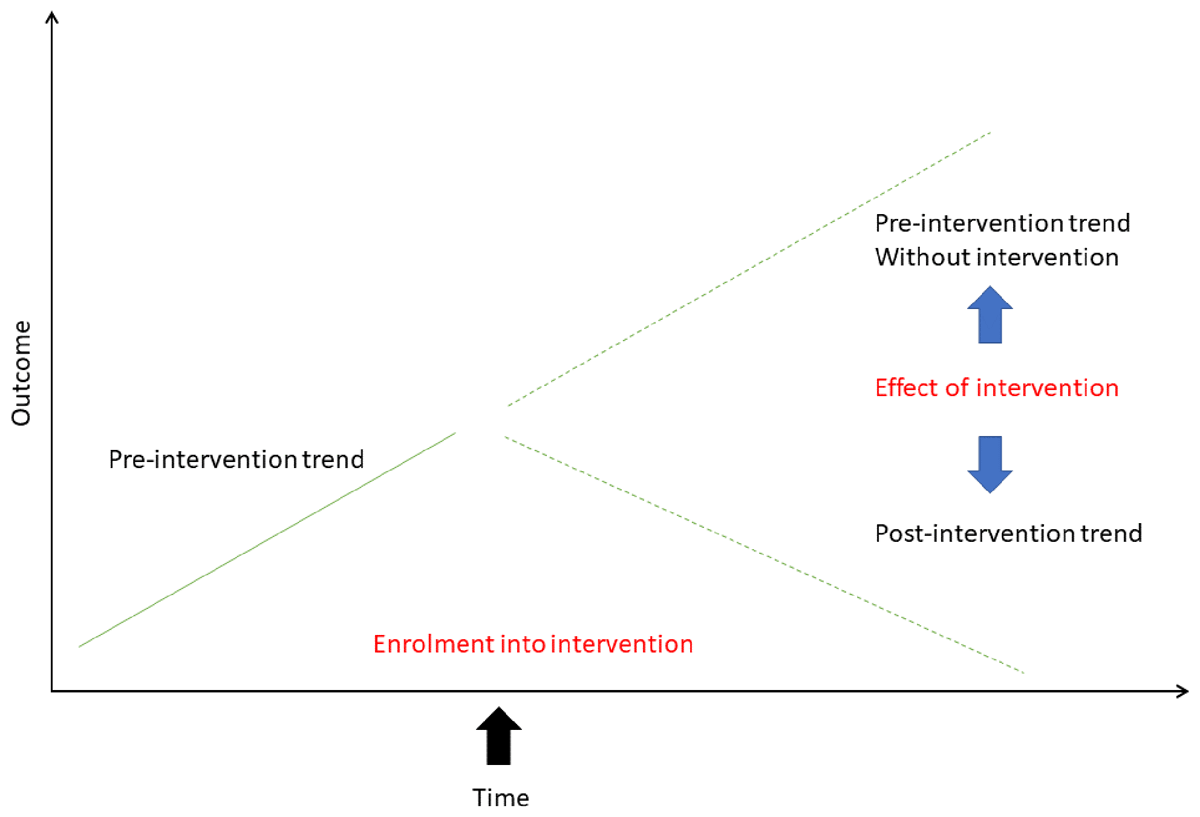
Figure 4
Using interrupted time series analysis to measure change before and after intervention. Adapted from Kontopantelis et al 2015 [13].
Table 2
Defining implementation outcomes for RuralKidsGPS, based on Proctor’s framework.
| OUTCOME | QUESTION |
|---|---|
| Acceptability | Do clinician and non-clinicians, parents and children view RuralKidsGPS as agreeable? |
| Adoption | To what extent do clinicians and parents use RuralKidsGPS? |
| Appropriateness | Do all stakeholders perceive RuralKidsGPS as relevant & useful? |
| Fidelity | Is RuralKidsGPS applied as intended? Are all component parts of the intervention delivered as planned? |
| Feasibility | Are the component parts of RuralKidsGPS practical to deliver within the service? |
| Coverage | How many service users of those eligible are reached? |
| Cost* | How much does it cost to successfully implement RuralKidsGPS? |
| Sustainability | What are the factors that will allow RuralKidsGPS to be scaled-up further? |
[i] *This outcome will be informed by the economic evaluation.
Table 3
Quantitative data collection for children and families, clinician and non-clinicians at each of the four sites.
| GROUP | INSTRUMENT | BASELINE (ENROLMENT) | 6 MONTHS | 12 MONTHS |
|---|---|---|---|---|
| Families | Paediatric Integrated Care Survey [6] | x | x | x |
| Clinician and non-clinicians | Intervention Acceptability, Appropriateness and Feasibility measure [15] | x | x | x |
| Clinicians and non-clinicians | NoMAD (Normalization Process Theory tool) [17] | x | x | |
| Clinician and non-clinicians | Routinisation and sustainability of work practices in long term care [18] | x |
Table 4
Sources, measures, and tools for evaluation.
| RESEARCH QUESTION | DATA SOURCE |
|---|---|
| 1. What is the impact of RuralKidsGPS on health service use? | Linked data from multiple sources Figure 3 |
| 2. What is the impact of RuralKidsGPS on family reported experiences, and parental satisfaction with care and care coordination? | Paediatric Integrated Care Survey [6] |
| 3. What is the family impact related to the child’s healthcare needs (travel and accommodation costs, care for siblings, missed work, missed school days)? | Adapted Mumford Survey [7]. |
| 4. What is the impact of RuralKidsGPS on parent and child related Quality of Life? | Parents: EQ-5D-5L [8] Children aged <7 years: Parent reported Paediatric Quality of Life Inventory [9] CYP aged 7–17 years: CHU9D [10] |
| 5. What is the impact of RuralKidsGPS on Parental mental wellbeing? | Warwick-Edinburgh Mental Well-being scale [11] |
| 6. What is the cost of implementing the model of care? What is the cost effectiveness? | Average costs per encounter in health service use (ED presentation, hospital admission, outpatients encounter); family cost estimates according to adapted method of Mumford et al., 2018 [7]; Quality adjusted life-years (QALYs) |
| 7. What are the aspects of the model of care and its implementation that support feasibility, acceptability and contextual appropriateness? | Qualitative semi-structured interviews guided by the Consolidated Framework for Implementation Research [25]; and the Proctor Implementation Outcomes Framework [15]. |
| 8. What are the barriers and enablers for implementing the model at scale? | Qualitative semi-structured interviews guided by the Consolidated Framework for Implementation Research [25]; and the Proctor Implementation Outcomes Framework [15]. |
| 9. What are the factors that will allow RuralKidsGPS to be scaled-up further? | Survey for healthcare professionals, researchers and health care managers that includes validated tools: Short intervention acceptability, appropriateness, and feasibility measure [15], Normalization Process Theory Nomad Tool [17], Routinisation and sustainability of work practices in long term care [18]. |
