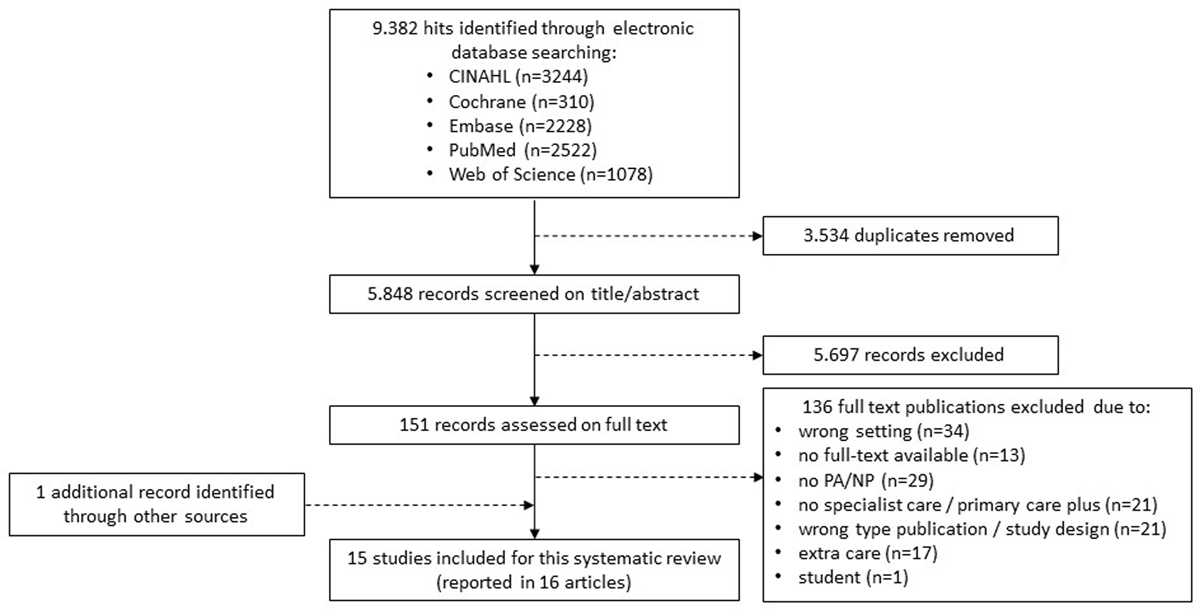
Figure 1
Study flow diagram.
PA = physician assistant, NP = nurse practitioner.
Table 1
Characteristics of the included studies.
| STUDY | COUNTRY | DESIGN | PARTICIPANTS | EDUCATION/RIGHTS | SPECIALIZATION | PRIMARY CARE PLUS | CONTROL INTERVENTION | AI |
|---|---|---|---|---|---|---|---|---|
| Ansari et al. (2009) | UK | Observational cohort study | NP (a team) | N.R. | COPD | Urgent Care Team (a team of NPs) provides ‘hospital-at-home’ to patients with an acute exacerbation of COPD. NP treats patients with nebulized bronchodilators, prednisolone and doxycycline. Support: N.R. | Usual hospital care | Preventing referral |
| Bookbinder et al. (2011) | USA | Descriptive study | NP (n = 1) | Advanced training in palliative care | Palliative care | Palliative home care team (secondary care NP and social worker) provides consultation and direct home care for homebound elderly with advanced illnesses. Support: Department of Pain Medicine and Palliative Care (nursing, social work, and medicine). | N.A. | Preventing referral |
| Gunn et al. (2000) | New Zealand | RCT | NS (a team) | Specially skilled nurses with neonatal nursing experience | Preterm infants | Team of NSs provides home support for preterm infants (daily home care visits for 7–10 days after early discharge, including weekends), and are 24h a day availably by telephone. Support: N.R. | Routine care; hospital care and daily standard home care including home visits/telephone contact by home care nurses for 5 weekdays after discharge. | Early discharge |
| Jack et al. (2008) | UK | Descriptive study | CNS (n = 1) | CNS does not prescribe opiate substitutes | Hepatitis C virus (HCV) | CNS in hepatitis forms a partnership with drug workers and GPs in a general practice. The CNS provides HCV consultations (screening, diagnosing and treatment). Supervision: secondary-care-based consultant in infectious diseases. | N.A. | Preventing referral |
| Kemp, A.E. (2016) | UK | Observational study | ANP (n = 1) | An independent prescriber and accredited prehospital care practitioner; have master’s level post-registration qualifications. | First aid | ANP works alongside an event medical team (paramedics and first aiders) at a mass-gathering event. ANP assesses, diagnoses, and provides treatments and advice (e.g. wound closures, prescribe medication). Support: N.R. | Usual care provided by the event medical team (without ANP). | Preventing referral |
| Lemelin et al. (2007) | Canada | Descriptive study | NP (n = 6) | Licensed as extended class RN’s; educated as Primary Care NP’s | Family Medicine | NPs provide daily home visits and telephone contact. The NPs performs physical examination and initiates care provision; rehabilitative and supportive care, including education, coordination of services, and counseling. Support and supervision: Family Medicine physicians. | N.A. | Preventing referral |
| Lucatorto et al. (2016) | USA | Pilot study, Pre–post, single-patient group design | NP (n = 1) | Nurses with advanced training and scopes of practice that include diagnosing disease and prescribing treatment | Diabetes and chronic kidney disease | Advanced Practice Registered Nurse (APRN)-Led Specialty Care Team for patients with diabetes and chronic kidney disease. The APRN-team consists of a NP, RN, licensed PN, RN certified diabetes educator, registered dietitian and clinical pharmacist. NP provides clinical examination and medication adjustment, is responsible for communicating the team plan, treatment changes, and summary of care to the primary care provider. Support: virtual technology and clinical decision making tools. | N.A. | Preventing referral |
| Lukas et al. (2013) | USA | Pre–post, single-group design | NP (n = 3) | N.R. | Palliative care | Physicians and NPs within a palliative medicine practice for elderly with advanced complex illness. Outpatient arm provides home-based, non-hospice palliative medicine consultation and management. NPs deliver direct care, e.g. symptom management, advanced care planning, goal-directed care and care coordination. Support: collaborating physician (20%). | Usual care (situation prior to the introduction of the palliative medicine practice) | Preventing referral |
| Maruthachalam et al. (2006) | UK | Observational study | NS (n = 1) | N.R. | Flexible sigmoidoscopy | Flexible sigmoidoscopy clinic developed at GP practice. Secondary care personnel delivers care; nurse endoscopist, colorectal nurse specialist, endoscopy nurse and auxiliary nurse. The colorectal NS manages benign conditions (e.g. haemorrhoids and anal fissures), provides verbal and written advice, books follow-up appointments. Support: protocols, contact with physician, weekly meetings to review patients (lead consultant and nurse endoscopist). | Secondary care | Preventing referral |
| McCorkle et al. (2000) | USA | RCT | APN (multiple) | Masters-prepared clinicians | Post-surgical cancer | APNs deliver 4-week specialized home care to post-surgical older patients with cancer (3 home visits, 5 telephone contacts). APNs provide education (43%), assessment and monitoring health status (25%), psychological support (16%), referrals (11%), others (5%). APNs are 24/7 available. Support: standardized protocol, physicians. | Usual post-operative hospital care and routine follow-up care in an ambulatory setting | Early discharge |
| McLachlan et al. (2015) | New Zealand | Cohort study (descriptive) | NP (n = 1) | NPs can practice autonomously or as part of team, and have prescribing rights | Post-surgical heart valve | NP-led clinic in community-based ambulatory care setting for patients following valve repair/replacement who require long-term follow-up. NP assesses patients annually/biannually, prepares review letter. Support and supervision: senior cardiologist (patient reviewing). | N.A. | Preventing referral |
| Moore, J.A. (2016) | USA | Pre-post, single-group design | NP (n = 2) | Depending on state: license for prescribing rights and full practice authority | Congestive heart failure | NP-led home-based clinic pathway for patients with congestive heart failure (5 days/week home visits, tele monitoring and weekly telephone contacts). Interdisciplinary team is involved including NPs, RNs, physiotherapists, occupational therapists, a dietician, pharmacists, social workers, and home health aides. NP provides history assessments, physical assessments, education, reconciles medication, reviews clinical pathway and CHF self-management tool, teaches and reviews tele monitoring equipment, and reviews tele monitoring data and follow-up. Support is not reported. | Usual care (situation prior to the introduction of the clinic pathway) | Preventing referral |
| Regan & Morgan (2015) | UK | Descriptive study | ANP (n = 2) | N.R. | Intravenous antibiotic service | Community-based service by two ANPs and core district nursing service for patients requiring IV antibiotics. ANPs assess patients, visits patients at home, functions as clinical leads and coordinators, promote the service in secondary care, and provide training and support for the district nursing team. Consultant in secondary care keeps final responsibility for patients. Support: radiologist, microbiologists and pharmacists. | N.A. | Early discharge |
| Tozer & Lugton (2007) | UK | Descriptive study | NS (n = 2) | N.R. | Genetic cancer screening | Nurse-led community service for people concerned about cancer. NS assesses the level of familial cancer risk, triages and refers patients, writes personalized letters, and provides advice. Support: innovative software. | N.A. | Preventing referral |
| Whitaker et al. (2001) | UK | RCT | NP (n = 1) | N.R. | Botulinum toxin injection for Dystonia | NP provides botulinum toxin injections at home. NP is allowed to make external medical, nursing, or therapy referrals. Support: clinical doctors. | Usual care (injections provided by medical staff in the outpatient clinic) | Preventing referral |
[i] NP = nurse practitioner; COPD = Chronic Obstructive Pulmonary Disease; N.R. = not reported; N.A. = not applicable; NS = nurse specialist; RCT = Randomized Controlled Trial; CNS = clinical nurse specialist; ANP = advanced nurse practitioner; APN = advance practice nurse; RN = registered nurse; PN = practice nurse.
Table 2
Risk of bias assessment.
| STUDIES | QUESTION | STUDY DESIGN | SELECTION | SUBJECT CHARACTERISTICS | RANDOM ALLOCATION | BLINDING INVESTIGATORS | BLINDING SUBJECTS | OUTCOME | SAMPLE SIZE | ANALYTIC METHODS | ESTIMATE OF VARIANCE | CONFOUNDING | RESULTS | CONCLUSION | SUMMARY SCORE* |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ansari et al. (2009) | 2 | 1 | 1 | 2 | n/a | n/a | n/a | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 18/22 = 0.82 |
| Bookbinder et al. (2011) | 1 | 1 | 1 | 2 | n/a | n/a | n/a | 2 | 1 | 2 | 2 | 1 | 2 | 2 | 17/22 = 0.77 |
| Gunn et al. (2000) | 2 | 2 | 2 | 2 | 2 | n/a | n/a | 2 | 1 | 2 | 0 | 2 | 2 | 2 | 21/24 = 0.88 |
| Jack et al. (2008) | 1 | 1 | 1 | 1 | n/a | n/a | n/a | 1 | n/a | n/a | n/a | n/a | 1 | 0 | 6/14 = 0.43 |
| Kemp, A.E. (2016) | 2 | 2 | 2 | 1 | n/a | n/a | n/a | 2 | 1 | 2 | n/a | 0 | 2 | 1 | 15/20 = 0.75 |
| Lemelin, J. et al. (2007) | 2 | 2 | 1 | 2 | n/a | n/a | n/a | 1 | n/a | n/a | n/a | n/a | 2 | 1 | 11/14 = 0.79 |
| Lucatorto et al. (2016) | 0 | 1 | 1 | 1 | n/a | n/a | n/a | 1 | n/a | n/a | n/a | n/a | 1 | 0 | 5/14 = 0.36 |
| Lukas et al. (2013) | 2 | 2 | 2 | 2 | n/a | n/a | n/a | 2 | 1 | 2 | 1 | 2 | 2 | 1 | 19/22 = 0.86 |
| Maruthachalam et al. (2006) | 1 | 2 | 2 | 1 | n/a | n/a | n/a | 1 | 1 | n/a | n/a | n/a | 2 | 1 | 11/16 = 0.69 |
| McCorkle et al. (2000) | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 23/28 = 0.82 |
| McLachlan et al. (2015) | 2 | 2 | 1 | 2 | n/a | n/a | n/a | 2 | n/a | 2 | 2 | 0 | 2 | 2 | 17/20 = 0.85 |
| Moore, J.A. (2016) | 2 | 1 | 1 | 1 | n/a | n/a | n/a | 2 | 0 | 1 | 2 | 0 | 2 | 2 | 14/22 = 0.64 |
| Regan & Morgan (2015) | 1 | 1 | 0 | 0 | n/a | n/a | n/a | 0 | 0 | n/a | n/a | n/a | 0 | 2 | 3/16 = 0.19 |
| Tozer & Lugton (2007) | 1 | 1 | 0 | 0 | n/a | n/a | n/a | n/a | n/a | 0 | 0 | n/a | 0 | 1 | 3/16 = 0.19 |
| Whitaker et al. (2001) | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 25/28 = 0.89 |
[i] * Total sum = (number of “yes” * 2) + (number of “partials” * 1); total possible sum = 28 – (number of “n/a” * 2); summary score = total sum/total possible sum.
Table 3
Outcomes of the included studies.
| STUDY | PATIENT OUTCOMES (MORBIDITY, MORTALITY, HEALTH STATUS, QUALITY OF LIFE, PATIENT SATISFACTION, PATIENT COMPLIANCE, AND PATIENT SAFETY) | PROVIDER OUTCOMES (JOB WORKLOAD, JOB SATISFACTION, AND THE EXPERIENCES OF PAS/APNS) | COSTS AND COST-EFFECTIVENESS (INCLUDING UTILIZATION OF RESOURCES) | CARE OUTCOMES (HEALTH CARE ACTIVITIES/ROLES SUCH AS EXAMINATION, ADVICE, TREATMENTS; THE QUALITY OF THE HEALTH CARE; AND FACILITATORS AND BARRIERS) |
|---|---|---|---|---|
| Ansari et al. (2009) | Health status FEV1% pred. (intervention) baseline: 46.9 ± 19.8, follow-up: 48.1 ± 21.6; FEV1% pred. (comparison) baseline: 45.9 ± 19.0, follow-up: 53.5 ± 18.2. Admission 1/60 patients in the intervention group (UCT) required admission to hospital within 10 days. | – | – | |
| Bookbinder et al. (2011) | Health status N = 45 sign. reduction in physical symptom subscale score (z = –2/390, p = 0.003). Admission N = 27 (22%) referred from the intervention to hospice. N = 32 active cases transitioned to other services for continued care. | – | Costs APN 350 visits ($67,000 total yearly reimbursement), 140 first time visits ($238 per visit), 17 inpatient visits ($300 per visit), 193 follow-up visits ($102–170 per visit) | Barriers Obtaining services, reimbursement for NP, acquisition of new patients, geographic distribution of patients, no. of visits, medical management by the NP. |
| Gunn et al. (2000) | Health status Breastfeeding rate or amount, ns. Patient satisfaction Majority satisfied intervention (early discharge). Admission Re-admission to hospital: 6 wk.: 8.8% vs. 11.9%, p = 0.37; 6 mo.: 20.2% vs. 20.3%, p = 0.96. | – | – | |
| Jack et al. (2008) | Patient compliance Attendance rate intervention: >85% (usually <40%). Compliance with therapy was good. | – | – | – |
| Kemp, A.E. (2016) | Admission Referral to local health care resources: 0.03 (23; 3.5%) vs. 0.12 (105; 16.1%), p < .001). Referral to hospital: 0.02 (20; 3.2%) vs. 0.11 (91; 14%), p < .001). Ambulance transport to hospital rate: 0.01 (11; 1,7%) vs. 0.06 (47; 7,2%), p < .001). | – | Costs Estimated direct savings = £22,066. | |
| Lemelin, J. et al. (2007) | Patient satisfaction High levels of satisfaction = 88–100%. Preferred site = 63% at home, 37% hospital. Adverse events N = 0 adverse events or mortality. Admission N = 2 re-admitted to the inpatient service. | Experiences physicians Virtually all: at least satisfied with intervention. 88% = did not affect/affect in a positive way practice routine. Experiences NP All: very good quality of care. Majority: satisfied participation in decision-making. Some patients too ill for NP-profession, others not requiring NP-expertise. | – | Facilitators NP could act autonomously. Barriers No direct access to diagnostic tests and specialists, challenges in developing relationships, defining roles and establishing program ‘buy-in’ with medical staff. |
| Lucatorto et al. (2016) | Health status Hemoglobin A1c and eGFR stages remained stable. Medication Angiotensin-convertin enzyme inhibitors/angiotensin receptor blockers: 20% increase; cholesterol-lowering medication: 27% increase; insulin: 10% increase; NSAIDs: 7% decrease. | Experiences NP Self-perceived confidence (diabetes) = 6.2; self-perceived confidence (renal disease) = 4.7; past experiences was related to higher confidence levels. | – | Facilitators Printed materials, collaboration, teamwork, experience, expertise, benchmarking, chance to network. Barriers Diverse patients, time to get lab. data, complexity of setting up shared medical appointment, patient transport issues. |
| Lukas et al. (2013) | Admission Sign. reduction in: no. of hospitalization (p = 0.000, d = 0.75), no. of days in hospital (p = 0.000, d = 0.81), 30-day readmission (p = 0.02, OR = 1.66). No sign. reduction in: emergency department visits (ns, OR = 1.20). | – | Costs Sign. reduction in: total costs for hospitalisation (p = 0.000, d = 0.52), variable costs for hospitalisation (p = 0.000, d = 0.53) | – |
| Maruthachalam et al. (2006) | Patient satisfaction 99% = satisfied clinic service (n = 447), 76% = had service on time (n = 342). Patients were willing to be investigated: less anxiety, better facilities, easier access. Admission to flexible sigmoidoscopie Median time in clinic = 35 days (range 1–180), in hospital = 87 days (range NR). Admission to hospital after flexible sigmoidoscopy 72% referral (n = 716), 28% no referral (n = 284). | – | Costs Flexible sigmoidoscopy in clinic = £270; flexible sigmoidoscopy in hospital = £396 (including equipment, salary, capital costs, costs for consumables) | – |
| McCorkle et al. (2000) | Risk of death Adjusted hazard ratio 2.4; CI 1.33–3.12; p =.001. 2-year survival rate Early stage patients = 90.3% versus 87.6%, ns. Late stage patients = 67% versus 40%, p < 0.05. Quality of life No difference between intervention and usual care. Admission 32% intervention versus 27% usual care. | – | – | – |
| McLachlan et al. (2015) | Medication Sign. increase in aspirin use (p = 0.001), but not statin, angiotensin converter enzyme inhibitor, calcium channel blocker, beta blocker, thiazide and angiotensin receptor blocker (p>0.05). Adverse events 2% stroke (n = 9), 4% died (n = 18). Admission/referral 4% referred to cardiologist (n = 18), 1% redo valve surgery (n = 6), 1,5% required urgent admission (n = 7). | – | – | – |
| Moore, J.A. (2016) | Admission Intervention results in substantial reduction (–28%) in 30-day hospital readmission and emergency department visits. | – | – | Facilitators Daily interactions, tele monitoring, weekly interdisciplinary home health meetings, staff involvement, informative brochures. Barriers Lack of notification new patients, handwritten medical visit information, NP part-time availability, restrictive NP practice privileges. |
| Regan & Morgan (2015) | Patient satisfaction 1/8 patients stated: ‘This is an excellent idea. I feel a lot better in myself by being treated at home. I was in hospital for five wk., only needing one injection a day, and I was getting very frustrated. | – | Barriers Unpredictable, sporadic transfers to service, weekends and bank holidays, limited capacity and skills. Facilitators Multidisciplinary professional engagement, communication with medical lead, communication pathways, assessment, co-ordination and patient management. | |
| Tozer & Lugton (2007) | – | Experiences clinicians Clinicians: in favor of the revised pathway. Nurses: convinced of its value. PCT team: has potential to become cost effective. | – | Barriers Distance travelled per visit varied (range 2–99 miles). |
| Whitaker et al. (2001) | Effectiveness No sign. differences in efficacy, duration and no. of treatments. Time between injection and reinjection was lower in intervention (1.5 wk.) than usual care (3.8 wk.). Patient satisfaction Home service was preferred over usual care (p = 0.001), efficacy improved (p = 0.001). Adverse events Similar in both groups except for sign. less dysphagia (p = 0.018) in the home group (7 versus 24 occasions). Admission N = 1 (intervention) was referred back | – | Costs Total cost per visit was not sign. different between the home injection group ($36.90/£23.36) and clinic group ($79.00/£50.01). |
[i] FEV1 = Forced Expiratory Volume in the first second; NP = nurse practitioner.
